Urticaria: An Undertreated Disease
M3 India Newsdesk Sep 23, 2022
Urticaria, or hives (sometimes referred to as welts or wheals), is a common disorder, with a prevalence of approximately 20 per cent in the general population. In this article, the author describes the types of urticaria, its causes along with the treatment measures.
A typical urticarial lesion is an intensely pruritic, erythematous plaque. Urticaria can be present in persons of any age. It is mostly acute but can be chronic in 10% of patients. Always rule out other causes of urticaria before calling it idiopathic.
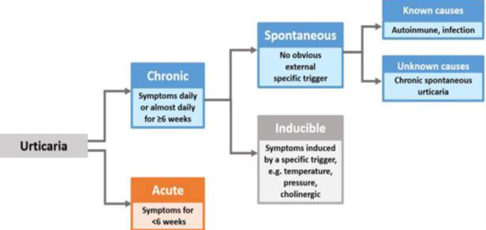
Types of urticaria
Urticaria, with or without angioedema, can be classified as acute or chronic. Urticaria that recurs within a period of fewer than six weeks is acute. Recurring chronic urticaria lasts longer than six weeks. Chronic spontaneous (idiopathic) urticaria (CSU), defined as the occurrence of wheals, angioedema, or both for more than 6 weeks, affects 1–2% of the population.
The lifetime prevalence for all types of urticaria is usually described below 10% per different reports, while chronic urticaria (CU) only develops in approximately one-fourth of these individuals.
Causes

There are various causes of urticaria. Common causes of new-onset urticaria include:
- Infections
- Allergic reactions to medications, foods, or insect stings and bites
- Reactions to medications that cause nonallergic mast cell activation (eg, narcotics)
- Ingestion of nonsteroidal anti-inflammatory drugs (NSAIDs)
Evaluation
The diagnosis of urticaria is usually clinical. The first step in evaluating urticaria and angioedema is a history and physical examination to characterize the lesions and help identify causes. History elements that should be elicited include onset, timing (e.g., with the menstrual cycle, if an association is suspected), location, and severity of symptoms; associated symptoms, which may suggest anaphylaxis; and potential environmental triggers.
Other important parts of the history include medication and supplement use, recent infections, travel history, family history of urticaria and angioedema, and a complete review of systems to identify possible causes and symptoms of systemic illnesses.
Wheals ls lasting longer than 24 hours, non-blanching papules, burning or other discomforts, residual hyperpigmentation, fevers, and arthralgias are classic features of urticarial vasculitis.
Diagnostic tests
Laboratory workup in the absence of indications of an underlying cause is not necessary. If the history or physical examination suggests a specific cause or underlying disease, targeted testing is appropriate. For example, a presentation that suggests urticarial vasculitis should prompt a skin biopsy, whereas if the history suggests an allergic trigger, allergy testing may be useful after the resolution of symptoms.
With chronic urticaria, or in acute cases if there are patient or parental concerns, a limited nonspecific workup including a complete blood count with differential, erythrocyte sedimentation rate and/or C-reactive protein testing, liver enzymes, and thyroid-stimulating hormone measurement can be considered to rule out underlying causes. When the history suggests physical urticaria, challenge testing with standardized physical stimuli can be done to confirm the diagnosis. Allergic testing is not recommended unless there is a specific indication.
Treatment
1. General measures
Patient interrogation and physical examination may disclose environmental symptoms triggering or aggravating factors of chronic urticaria (CU). When identified, it is mandatory to avoid or reduce exposure to such factors (physical, drugs: NSAIDs, ACE inhibitors, foods, other allergens, contacts, emotional stress).
2. Medications
If trigger avoidance is impossible, no trigger is identified, or symptom relief is needed despite trigger avoidance, H1-antihistamines are first-line pharmacotherapy. Second-generation H1 antihistamines such as loratadine (Claritin), desloratadine (Clarinex), fexofenadine (Allegra), cetirizine (Zyrtec), and levoceti-rizine (Xyzal) are relatively nonsedating at standard dosages and are dosed once per day.
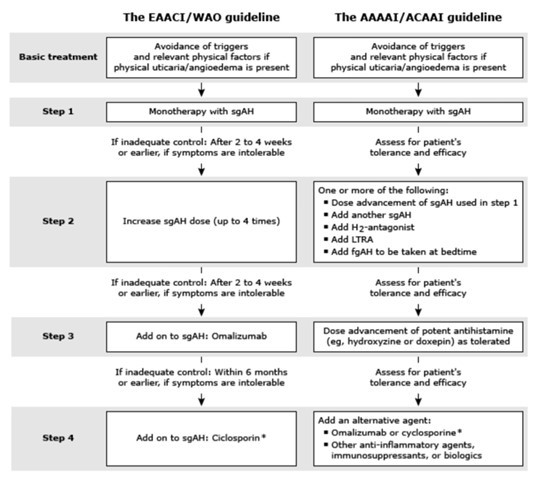
According to the guidelines given by EAACI first step is always to avoid allergens and triggering factors and start with antihistamines drugs. If no control with antihistamines after 2-4 weeks increase the dose of antihistamines up to 4times the usual dose. If still no control after 2-4 weeks add Omalizumab ( monoclonal antibody against IgE). Still, if still no control after 6months add cyclosporine to antihistaminics
3. Steroids
Glucocorticoids do not appear to be necessary for isolated urticaria. However, a brief course (ie, usually a week or less) of systemic glucocorticoids may be added to antihistamine therapy for patients with prominent angioedema or if symptoms persist beyond a few days. In adults – Prednisone 30 to 60 mg daily, with tapering of the dose over five to seven days can be given
4. Urticarial vasculitis(UV)
The urticarial plaques of UV last longer than those in chronic urticaria, persisting for more than 24 hours in two-thirds of patients, and sometimes for up to 72 hours. The urticarial plaques may resolve without a trace but may also be associated with residual purpura or hyperpigmentation in up to 35 per cent.
Diagnosis of urticarial vasculitis is made if the following two features are present:
- Clinical manifestations of urticaria
- Histopathologic evidence of cutaneous leukocytoclastic vasculitis (LCV) of the small vessels, largely involving the postcapillary venules
Laboratory parameters in UV:
- Elevated erythrocyte sedimentation rate (ESR)
- Hypocomplementemia (usually decreased C1q, C3, and C4)
- Circulating immune complexes by the C1q solid phase test and/or anti-C1q antibody assay.
- Positive antinuclear antibodies (ANA)
Management
Mild disease can be managed with antihistaminics (fexofenadine 60mg twice a day. Moderate disease activity Glucocorticoids with or without dapsone are typically used as initial therapy for patients with mild to moderate disease (no organ- or life-threatening disease manifestations such as renal failure) who have not responded to antihistamines and NSAIDs.
Other drugs which can be used are colchicine and HCQ.Severe disease for patients with refractory symptoms or those with organ-threatening or life-threatening disease manifestations.
Click here to see references
Disclaimer- The views and opinions expressed in this article are those of the author's and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr Radhika Jakhotia is a DNB resident in rheumatology from Manipal hospital.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries