Unraveling the Current Conjunctivitis Outbreak - Insights and Guidelines for Healthcare Professionals
M3 India Newsdesk Aug 10, 2023
The article explores the recent conjunctivitis outbreak causing red eye cases nationwide, detailing its types, symptoms, diagnosis, prevention, and treatment. Emphasises hygiene and seeking medical help.
Current outbreak
Conjunctivitis is one of the most prevalent causes of red eye, affecting people of all ages and socioeconomic backgrounds.
- Now in the last 7-8 weeks, it has been seen all over the country that the cases of the red eye have emerged like anything.
- Many peoples in homes and hospitals as well as patient attendants of the hospital also show symptoms of red eye.
- It has spread sudden havoc in society.
- And it has led to a scarcity of eye drops in the market.
So let’s understand what is conjunctivitis and what should be done and what should not be done.
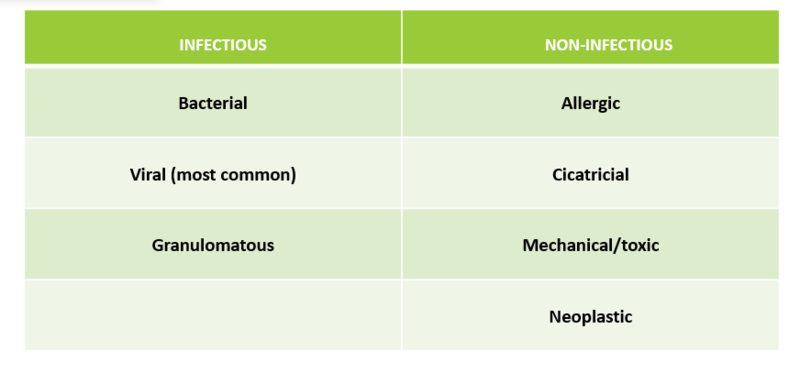
Definition and types of conjunctivitis
Conjunctivitis is an inflammation or infection of the translucent membrane that borders the eyelid and covers the white area of the eyeball (conjunctiva). When the conjunctiva's little blood vessels get irritated, they become more apparent. This is what causes the white of the eyes to appear reddish pink.
Conjunctivitis is the most common cause of red eye. It can be of various types like allergic, viral, and bacterial, the current outbreak is mostly viral.
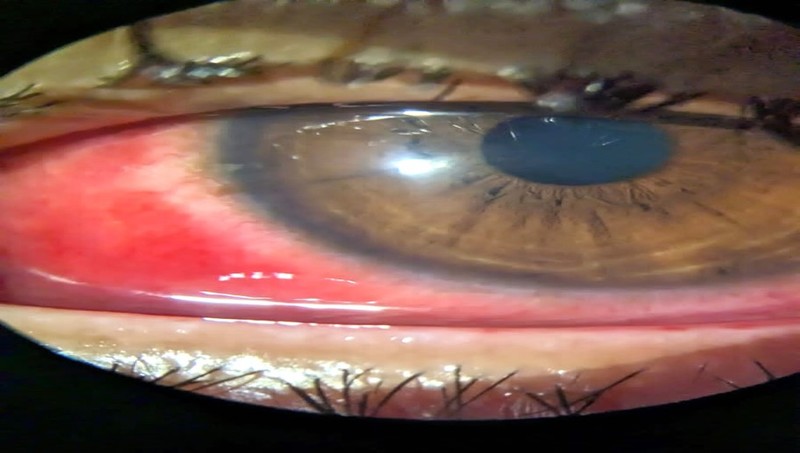
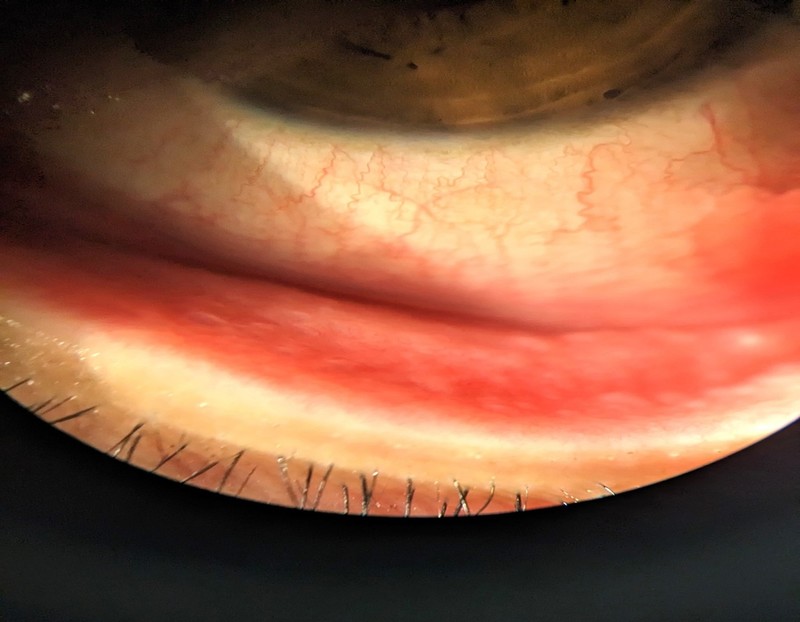
- Viral conjunctivitis-there is redness of eyes and periodic itching, increased lacrimation, tender preauricular lymphadenopathy, conjunctival hyperemia and follicles, subconjunctival haemorrhage.
- Allergic conjunctivitis- there is transient acute and sub-acute itching and redness of the eye, swelling of the conjunctiva and the eyelid, conjunctival papillary reaction, and ropy discharge.
- Bacterial conjunctivitis- redness, dryness of the eyes and the skin around them, mucopurulent discharge, lid oedema and erythema.
Clinical presentation
The hallmark sign of pink eye is the pink or reddish eye.
Other signs and symptoms include:
- Yellow or green mucous discharge
- Watery eyes
- Itchy eyes
- Increased sensitivity to light
- Pain (when there is corneal involvement)
Sometimes subconjunctival haemorrhage may occur.
Diagnosis
- The diagnosis is made clinically with a thorough history and classical physical examination findings.
- If there is any concern based on the history and physical examination, fluorescein staining of the cornea can ensure no corneal involvement.
- Conjunctival swabs for gram staining and culture sensitivity can be taken. As this outbreak is mostly due to viral aetiology with super-added bacterial infection, we can go for a PCR.
- And Giemsa stain to identify viral aetiology such as a mononuclear cell in adenovirus, and multinucleate giant cells in herpetic infection.
- Laboratory testing is generally not needed, although skin prick or serum allergy testing can help mitigate the disease process by identifying the offending allergens.
Differential diagnosis
- Allergic conjunctivitis
- NLD obstruction
- Trauma
- Corneal abrasion
- Uveitis
- Dry eye
- Blepharitis
Transmission and prevention
Both bacterial and viral conjunctivitis can be caused by airborne sources, so spread easily to others. Following preventive guidance should be given to the patients:
- It is spreading through direct contact with objects that are touched with the conjunctivitis eye.
- Washing hands frequently with soap.
- Personal items, including hand towels, should never be shared at the office and home.
- Don’t use a handkerchief, towel, pillow, or eye drop that has been used by a conjunctivitis patient.
- Wash your spectacles regularly.
- Avoid swimming pools and ponds.
- Contact lens users consult with their ophthalmologist and take prevention.
- Don’t use any abnormal things in the eye.
- If your patient has red eye then use a clean cloth and soak it with warm water and clean his eyes.
- And wash the cloth with warm water and detergent.
- If necessary go to a nearby hospital and consult an ophthalmologist.
Complications
- Sub conjunctiva haemorrhage
- Punctate keratitis with sub-epithelial infiltrates
- Bacterial superinfection
- Conjunctival scarring
- Symblepharon
- Severe dry eye
- Persistent keratoconjunctivitis
- Corneal scarring
Treatment approaches
- Spontaneous resolution of adenoviral infection usually occurs within 2-3 weeks so Most of the cases are treated symptomatically with NSAIDs and antihistamines like loratadine and vasoconstrictors (phenylephrine).
- Artificial tear drops (CMC eye drops).
- Cold compressions.
- Topical antibiotics such as moxifloxacin, gatifloxacin, and tobramycin can be given if superadded bacterial infection is suspected.
- Acyclovir ointments only if corneal involvement is there.
- And severe cases may need topical steroids.
- Discontinuation of contact lens use till resolution of symptoms.
Case studies
Case 1
A 34-year-old female from Bhubaneswar presented with complaints of bilateral lid swelling, redness and foreign body sensation, matting of eyelashes in the morning and watery discharge for 3 days.
Also patient was having a common cold for 5 days.
Diagnosis
- On examination, there was preauricular LN palpable on the left side.
- On slit lamp examination-conjunctival congestion was present, chemosis was present, and subconjunctival haemorrhage was present.
- Punctate haemorrhage and papillae were found on the upper palpebral conjunctive.
- Cornea was clear (flouroscein stain –negative) and the sensation was intact in all 4 quadrants of the cornea.
- The patient was diagnosed with a case of “viral conjunctivitis”.
Treatment
The patient was given tear substitute (CMC 0.5%) and olopatadine 0.2%, cold compression was advised and on follow up patient recovered from all the symptoms after 2 weeks.

Case 2
A 54-year-old man presented with watering from both eyes with itching, burning and redness in both eyes for 6 days.
Diagnosis
- On examination conjunctival congestion with follicles appreciated on the lower palpebral conjunctiva.
- With fluorescein stain cornea stained negative and there was an intact corneal sensation.
- The patient was diagnosed with a case of conjunctivitis of viral aetiology.
Treatment
The patient was given symptomatic management and the patient was explained about the personal hygiene method and prevention of transmission.

Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr Khemeswar Agasti is an MD in General Medicine from Cuttack.
Co Author-Dr. Manisha Mishra, MS ophthalmology, Cuttack.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries