Ulcerative colitis: How to tailor treatment as per AGA guidelines
M3 India Newsdesk Dec 16, 2021
Ulcerative colitis is a disease that negatively and gravely affects the lifestyles of patients. It is difficult to predict the prognosis of patients with UC. Clinicians need to study patient assessment and devise treatment plans to produce the best possible health outcomes. This article highlights the most important treatment updates from the American Gastroenterological Association (AGA).
Ulcerative colitis (UC) is a chronic idiopathic inflammatory bowel disease (IBD) of the colon that causes superficial mucosal inflammation in a continuous fashion extending from the rectum to the more proximal colon. It is characterised by a relapsing and remitting course. The hallmark symptoms of UC include bloody diarrhoea with rectal urgency and tenesmus.
Although the aetiology of UC remains a subject of debate, increasing evidence suggests the presence of an underlying autoimmune component. Many UC patients experience extraintestinal manifestations (EIM) that involve multiple organs sharing features with other autoimmune disorders.
UC is the most common in industrialised countries and the incidence has been rising in Asia. It is unclear how many Indians have Irritable Bowel Syndrome (IBD), but a 2017 study estimated that more than 1.1 million people had UC.
Risk factors
- UC has a bimodal age distribution with an incidence peak in the second or third decades of life followed by a second peak between 50 and 80 years of age.
- About 8-14% of patients with UC will have a family history of IBD, more commonly UC.
- Active smoking has a strong inverse association with active UC. A study confirmed that the risk of UC increased within 2–5 years after smoking cessation and remained elevated for 20 years after.
- Increased dietary intake of total fat, animal fat and polyunsaturated fatty acids has been correlated with an increased incidence of UC.
- Dysbiosis of the intestinal microbiota has been suggested as an important risk factor in IBD. However, the difference in microbial diversity is greater in Crohn’s disease than in UC.
- The mucosal transcriptional profile has shown a disordered interaction between the mucosa and microbiota in IBD.
Clinical features
- The classic presentation of UC includes bloody diarrhoea with or without mucus, rectal urgency, tenesmus, and variable degrees of abdominal pain that is often relieved by defecation.
- It may sometimes present with constipation.
- It may also present with anaemia, weight loss and bowel movements- more than 4 times a day.
Diagnosis
Clinical features
- Diarrhoea
- Abdominal pain
- Urgency
- Tenesmus
- Hematochezia
- Blood and mucus in the stool
Lab findings
- Inflammatory markers: Elevated erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), faecal calprotectin, and faecal lactoferrin.
- Nutrition markers: Low ferritin, anaemia, and low albumin levels.
Endoscopic findings
- Inflammation begins in the rectum and extends proximally in a circumferential and continuous fashion.
- Findings include erythema, oedema/loss of the fine vascular pattern, increased granularity of the mucosa, friability/spontaneous bleeding, pseudopolyps, erosions, and ulcers.
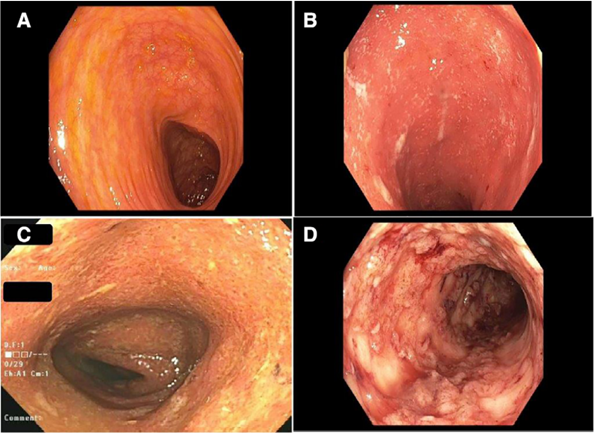
Colonoscopy images showing (A) normal colon, (B) mild colitis, (C) moderate colitis, (D) severe colitis
Histological findings
- Crypt abscesses, crypt branching, crypt shortening, crypt disarray, and crypt atrophy
- Mucin depletion
- Paneth cell metaplasia
- Increased lamina propria cellularity
- Basal plasmacytosis
- Basal lymphoid aggregates
- Lamina propria eosinophils
Differential diagnosis
| Symptom | Disease |
| Bloody diarrhoea | Behcet’s disease |
| Crohn’s disease | |
| Infectious colitis | |
| HIV/AIDS | |
| Neoplasms | |
| Ischaemic Colitis | |
| STD | |
| Radiation colitis | |
| Non-bloody diarrhoea | IBS |
| Crohn’s disease | |
| Pancreatic insufficiency | |
| Neoplasms | |
| Infections | |
| Hyperthyroidism | |
| HIV/AIDS |
Disease severity
Montreal classification of UC:
- S0 (clinical remission): No symptoms
- S1 (mild UC): Four or fewer stools per day (with or without blood), absence of systemic symptoms, normal inflammatory markers
- S2 (moderate UC): More than four stools per day, minimal signs of systemic symptoms
- S3 (severe UC): Six or more bloody stools per day, pulse rate of ≥90/min, Temp ≥37.5 °C, Hb less than 10.5 g/100 ml, and ESR of at least 30 mm/h
AGA treatment guidelines
One approach is never a perfect fit for a patient with ulcerative colitis (UC) and moreover, one patient may require multiple treatment modalities to achieve remission. It is also essential to be able to identify higher-risk patients, as their treatment approach may require more frequent and aggressive interventions.
The following treatment guideline is recommended by the American Gastroenterological Association (AGA) for UC:
- In adult outpatients with moderate-severe UC, the AGA recommends using infliximab, adalimumab, golimumab, vedolizumab, tofacitinib, or ustekinumab over no treatment.
- In adult outpatients with moderate-severe UC who are naïve to biologic agents, use infliximab or vedolizumab rather than adalimumab, for induction of remission. For patients who have previously been exposed to infliximab, particularly those with primary non-response, the AGA suggests using ustekinumab or tofacitinib, rather than vedolizumab or adalimumab for induction of remission.
- Induction/maintenance of remission:
- In adult outpatients with active moderate-severe UC, the panel suggests against using thiopurine monotherapy for induction of remission.
- In adult outpatients with moderate-severe UC in remission, it has been suggested to use thiopurine monotherapy, rather than no treatment, for maintenance of remission.
- In adult outpatients with moderate-severe UC, the panel suggests against using methotrexate monotherapy, for induction or maintenance of remission.
- In adult outpatients with active moderate-severe UC, the recommendation suggests using biologic monotherapy (TNF-α antagonists, vedolizumab or ustekinumab) or tofacitinib rather than thiopurine monotherapy for induction of remission.
- In adult outpatients with moderate-severe UC, combine TNFα antagonists, vedolizumab or ustekinumab with thiopurines or methotrexate, rather than biologic monotherapy and combine TNF-α antagonists, vedolizumab or ustekinumab with thiopurines or methotrexate rather than thiopurine monotherapy.
- In adult outpatients with moderate-severe UC, early use of biologic agents with or without immunomodulator therapy, rather than a gradual step up after the failure of 5-aminosalicylates is recommended.
- In adult outpatients with moderate-severe UC who have achieved remission with biologic agents and/or immunomodulators or tofacitinib, it is suggested against continuing 5-aminosalicylates for induction and maintenance of remission.
- In hospitalised adult patients with acute severe UC, the AGA panel suggests using intravenous methylprednisolone dose equivalent of 40 to 60 mg/d rather than higher dose intravenous corticosteroids.
- In hospitalised adult patients with acute severe UC without infections, the AGA suggests against adjunctive antibiotics.
- In hospitalised adult patients with acute severe UC refractory to intravenous corticosteroids, use infliximab or cyclosporine.
- In hospitalised adult patients with acute severe UC being treated with infliximab, the AGA makes no recommendation on routine use of intensive vs. standard infliximab dosing.
Click here to see references
Disclaimer- The views and opinions expressed in this article are those of the author's and do not necessarily reflect the official policy or position of M3 India.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries