Tuberculosis: Early diagnosis & clinical approach
M3 India Newsdesk Mar 24, 2022
This World TB Day we bring to you an article that aims to define the management of TB through early diagnosis and initiation of multidrug regimen, preventing the emergence of drug resistance and prevention of spread in the community.
Tuberculosis: Disease outline
Tuberculosis (TB), is a multisystem disease with varied presentations. Worldwide, it is one of the common causes of infectious disease-related mortality. The incidence of TB is less in developed countries however; it is increasing in many developing and underdeveloped countries. In addition, globally the prevalence of drug-resistant TB is rising .
- Early diagnosis is crucial for successful management. The condition is diagnosed using a combination of clinical, radiographic, microbiological, and histopathologic investigations.
- Early initiation of appropriate multidrug therapy is the hallmark for effective management.
- In addition to efficient management of patients with active TB, preventive strategies are vital for the containment of the disease.
- Public health management strategies include contact investigation and testing of people in close contact with patients with active TB.
- Targeted testing and treatment is beneficial to reduce the burden of TB in the population [1].
The burden of TB in India
Worldwide, India has the highest prevalence of TB with approximately 35-40 crores of people affected with TB. It is estimated that the annual incidence of TB in India is around 18-36 lakh [2]. Thus, India has a very high burden of TB and appropriate management is vital to overcome it.
Mode of transmission
TB is of two types, namely pulmonary TB and extrapulmonary TB. Pulmonary TB is more common and is highly infectious [3]. It is transmitted by airborne droplets [4]. Patients with cavitary lesions or positive acid-fast bacilli smears are the most contagious; nevertheless, patients with negative smears but positive cultures can still be transmissible [1]. It is reported that annually each untreated smear-positive pulmonary TB patient can infect 10-15 people [4].
Clinical manifestation
Symptoms are insidious in the onset and the commonest presentation include:
- Low-grade fever
- Cough
- Weight loss
- Fatigue
- Night sweats
Uncommon symptoms include:
- Chest pain
- Dyspnea
- Hemoptysis
Physical examination findings could be rales or signs of pleural effusion (eg, dullness to percussion) [1].
Diagnostic tools for TB
The diagnostic tools for pulmonary TB include sputum smear microscopy, culture and chest X-ray.
- Sputum smear microscopy is the key method that can be used for diagnosis and monitoring the condition of the patient. It is estimated that at least 50% of newly diagnosed patients with pulmonary TB will have a positive smear. [2] sputum samples should be collected on 2 consecutive days and subjected to microscopic examination.
- Chest X-ray is used as an adjunct to microscopy.
- The culture of mycobacterium tuberculous bacilli has high sensitivity and specificity. However, it has several disadvantages such as high cost, the requirement of specialised laboratory setting and non-availability of immediate test results. Therefore, culture and sensitivity testing is mainly restricted for the diagnosis and management of drug-resistant tuberculosis, for epidemiological surveillance and planning and to ensure a relapse-free cure[4,5].
The following flow chart is recommended as per Indian guidelines for the diagnosis of TB (figure 1)6.
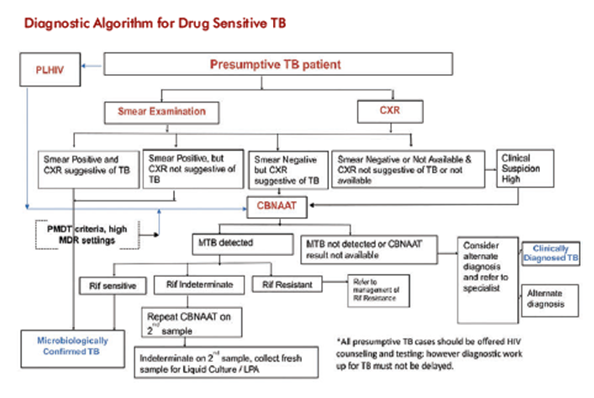
Figure 1: Indian guidelines for the diagnosis of TB [5]
Goals of treatment
The following are the aims of TB treatment [4,5,6]:
- Make the patient non-infectious
- Break the chain of transmission
- Decrease prevalence of infection
- Reduce TB related mortality and morbidity
- Ensure relapse-free cure
- Minimise and prevent emergence and progression of drug resistance
- Minimise the side effects of anti-tuberculosis drugs
Management of TB
The TB treatment as per the National tuberculosis elimination programme (NTEP) guidelines recommends a daily regimen since relapse rates are higher with intermittent regimen [5]. Treatment consists of intensive phase (IP) with 4 drugs and continuation phase with fewer drugs. The standardized anti-TB treatment is as follows (table 1) [5]:
| Type of patient | Treatment regimen |
|
Drug sensitive tuberculosis |
2HRZE+ 4HRE |
| Extrapulmonary tuberculosis |
2HRZE+ 4HRE IP can be increased to 3- months (TB meningitis, bone, joint, spinal TB) |
Table 1: Anti-TB treatment [5]
The number before the letter denotes the number of months of treatment; I: Isoniazid (5mg/Kg daily); R: Rifampicin (10mg/Kg daily); P: pyrazinamide (25mg/Kg daily); E: ethambutol (15mg/Kg daily) S: streptomycin (15mg/Kg daily)
As per the NTEP guidelines, directly observed treatment (DOT) is a key element for TB management. As per DOT, the patient takes the treatment under the supervision of an observer. This ensures that the patient continues the treatment and completes the prescribed course with the correct drugs, in the right doses and at right intervals [4,5]. The patient is declared cured if the conditions presented in table 2 are met [4].
| Patient characteristics | Treatment outcome |
| Microbiologically confirmed TB patients completed treatment and had negative smear or culture results | Cured |
|
Microbiologically confirmed TB patients, completed treatment with positive smears at the end of IP but no resistance to H and R detected or with negative smears at end of the intensive phase, but none at the end of treatment. Clinically diagnosed patient, pulmonary or extrapulmonary completed treatment with no positive smear or culture at the end of treatment |
Treatment completed |
Table 2: Treatment completion [5]
Management of multi drug-resistant (MDR) TB
As per world health organisation (WHO) guidelines, the drugs for management of MDR-TB are classified in 3 groups depending on the efficacy, experience of use and drug class (table 3) [5].
| Groups and steps | Drug |
| Group A: Include all three drugs |
Levofloxacin or Moxifloxacin Bedaquiline Linezolid |
| Group B: Add one or both drugs |
Clofazimine Cycloserine or Terizidone |
| Group C: Add to complete the regimen and when drugs from groups A and B cannot be used |
Ethambutol Delamanid Pyrazinamide Imipenem-cilastatin or meropenem Amikacin or streptomycin Ethionamide or prothionamide p-aminosalicylic acid |
Table 3: Grouping of anti-TB drugs for MDR-TB [6]
Prevention of TB
The primary aim of TB control is the treatment of patients with active TB, followed by a contact investigation of all people who came into close contact with the patients before the beginning of therapy.
Such contact investigation is recommended for all patients with confirmed active pulmonary TB and on selected patients with suspected pulmonary TB before testing is complete. Since patients with extrapulmonary TB are usually not infectious, contact investigation is not recommended [1]. The following guidelines enable control of TB in the population [2,4]:
- Promotion of awareness in the population, including medical professionals regarding the suspicious symptoms of TB
- Contact investigation of household contacts of smear-positive TB patients
Health education
Health education and counselling for the patients and caregivers about the disease, the mechanism of transmission and the need of taking regular and adequate treatment is of utmost importance. Effective counselling at the time of treatment initiation has been shown to be successful in the prevention of the development of drug resistance. Counselling should be started at the initial point of contact soon after the establishment of the diagnosis and should be continued during all visits by the patient to a health centre and also by the healthcare workers to the patients’ home or through the national TB call centre [6].
Click here to see references
Disclaimer- The views and opinions expressed in this article are those of the author's and do not necessarily reflect the official policy or position of M3 India.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries