Sudden loss of vision for an otherwise healthy individual
M3 India Newsdesk Feb 15, 2023
Sudden visual loss requires immediate attention. It is essential to identify whether the visual loss is due to optic neuropathy or an ocular disorder like a retinal disease. The following article elaborates on these conditions with the basis of some case studies.
Case 1
A 30-year-old female patient came to OPD and appeared healthy.
On Examination
- No h/o eye pain, discharge, headache, double vision, history of trauma, systemic illness, family history or addictions.
- Her visual acuity was 6/24 in the right eye and 6/6 in the left.
- Their pupils were normal in size and shape but she had a mild afferent pupillary defect in his right eye.
- There was no ptosis or lid retraction.
- Eye movements in the right eye had mild pain. Anterior segment evaluation was normal with normal intraocular pressures.
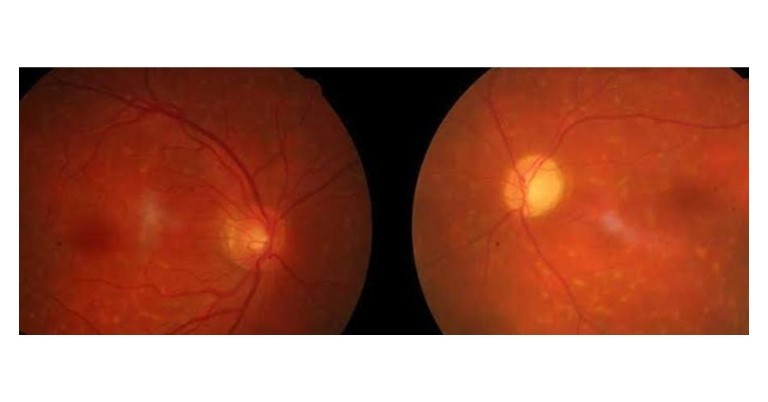
- On the temporal side of the right optic disc, his dilated exam revealed a focused circular patch of elevation that masked the nerve's border.
- Oedema spread temporally from the nerve towards the macula. The vessels and periphery appeared normal. The left eye was normal.
Diagnosis and conclusion
On further evaluation, visual field examination revealed scotoma, impaired colour vision, contrast sensitivity and abnormal visual evoked potentials. MRI was under normal limits. The Fundus picture and the rest of the positive findings are suggestive of optic neuritis.
Case 2
A 19-year-old female presented for a routine eye check-up.
On Examination
- The patient had been getting increasing headaches which she thought were a result of her driving and studying frequently.
- On history taking, there were no other health issues or medications.on clinical examination, a vision was RE: 6/6 and LE: 6/9.
- Ocular motility was Full and smooth with no double vision and there was a sluggish pupillary reaction in both eyes.
- On the Posterior segment examination, there was significant bilateral swelling with haemorrhages over peripheral optic discs.
- Macula and were oedematous n both eyes with hard exudates collection suggestive of ischemic changes.
Diagnosis and conclusion
There were signs of bilateral optic nerve swelling and her symptoms of increased headaches, where an urgent MRI scan of the head and orbits was taken. As symptoms of papilloedema, MRI scans may reveal enlarged optic nerves, a flattened posterior globe appearance, and occasionally protruding optic nerve heads.
Discussion
Causes of sudden painless vision loss in an otherwise healthy individual
- Central retinal arterial occlusion
- Central retinal venous occlusion
- Papilloedema
- Central serous retinopathy
Causes of sudden painful vision loss in an otherwise healthy individual
- Optic neuritis
- Acute congestive glaucoma
Differential diagnosis and investigations
The evaluation of a patient with acute visual loss begins with a careful history. Details from the patient's description of visual symptoms may offer a preliminary suggestion of whether visual loss results from ocular or optic nerve pathology. Metamorphopsia and flashing or coloured lights often indicate a retinal lesion. Conversely, visual blurring with a description that colours look “washed out” or “faded” may suggest optic nerve dysfunction.
The amount of visual loss gives important clues regarding the potential aetiology: for example, in patients with optic neuritis it may quickly evolve and then subsequently improve; in ischemic optic neuropathy it may be sudden and fairly static; in patients with compressive lesions, its discovery may be sudden, but it is slowly progressive. In addition, it is important to elicit the presence or absence of associated orbital, neurologic, or systemic symptoms. The quality and severity of pain should be characterised; pain is typically present in disorders such as optic neuritis or giant cell arteritis, but is absent in most retinal diseases or nonarteritic ischemic optic neuropathy.
A detailed examination is necessary. When acuity cannot be improved by a pinhole or refraction, optic nerve and ocular disorders that can both cause reduced central visual acuity must be taken into account. Colour vision is often disproportionately affected by optic neuropathy. The Amsler grid, which is a series of horizontal and vertical lines similar to graph paper, may have an abnormal appearance to a patient with macular disease.
Visual fields can be assessed through confrontation techniques, but detailed perimetry testing is more sensitive and can reveal patterns of field loss that suggest a specific localisation and differential diagnosis.
Although it usually happens with optic neuropathy, depression of the central visual field is expected with maculopathy. Conversely, a “nerve fibre bundle field defect” is more specific for optic neuropathy. Finally, the examination of visual fields may also reveal homonymous field loss caused by a retro chiasmal lesion, even when the patient believes the vision alteration to be monocular of visual fields may identify homonymous field loss owing to a retro chiasmal lesion, despite the patient's misperception that the change in vision is monocular. MRI can be useful in separating inflammatory, ischemic, and neoplastic optic neuropathies.
Optical coherence tomography (OCT) provides high-resolution cross-sectional images of the retina that aid in distinguishing retinal pathology from optic neuropathy. Fluorescein angiography is used in some cases where there is suspicion of occult maculopathies, such as an ischemic lesion associated with diabetes.
1. Central Retinal artery occlusion: It is characterised by retinal whitening with a macular cherry-red spot. In the case of a branch retinal artery occlusion. A difference between the retina's afflicted and spared portions is made in the event of a branch retinal artery obstruction between affected and spared areas of the retina.
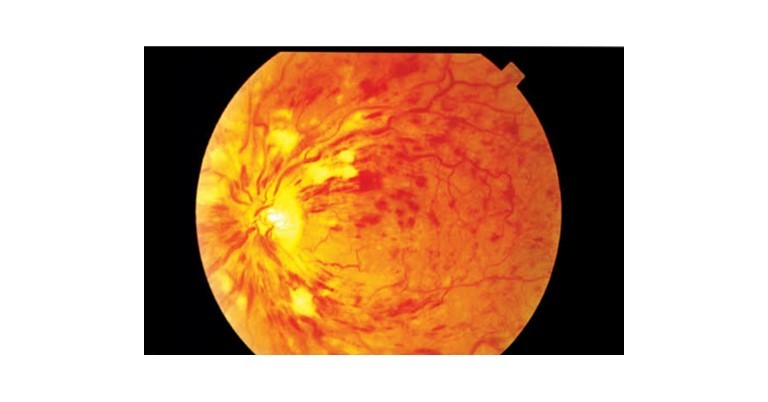
 2. Central Retinal vein occlusion: It produces multiple small retinal haemorrhages and engorgement of retinal veins. Retinal detachment, which produces a profound visual loss when the macula is involved, is identified by the observation of abnormal retinal elevation.
2. Central Retinal vein occlusion: It produces multiple small retinal haemorrhages and engorgement of retinal veins. Retinal detachment, which produces a profound visual loss when the macula is involved, is identified by the observation of abnormal retinal elevation.
 3. Cystoid macular oedema: Reduced acuity is another effect of cystoid macular oedema. On dilated fundus examination, the macula may appear mildly thickened or elevated, but on OCT, it is easy to see.
3. Cystoid macular oedema: Reduced acuity is another effect of cystoid macular oedema. On dilated fundus examination, the macula may appear mildly thickened or elevated, but on OCT, it is easy to see.
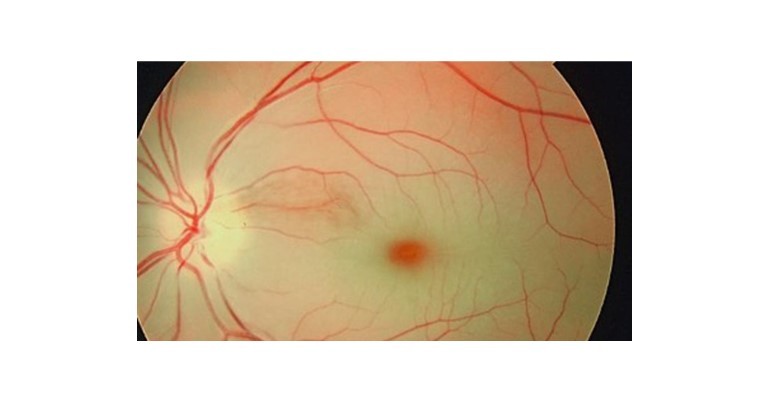
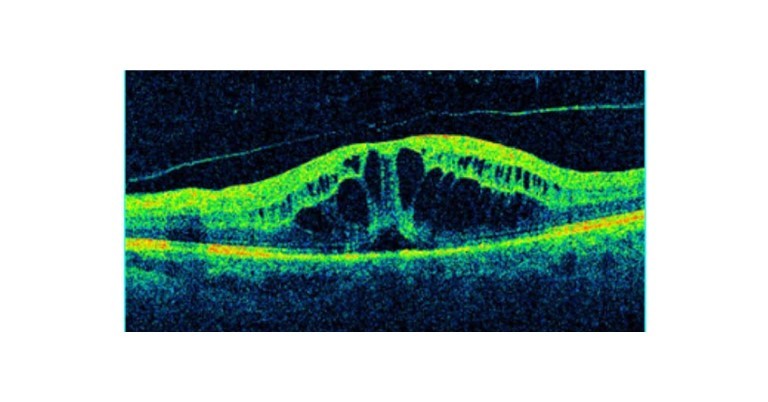 4. Central serous retinopathy: Due to macular subretinal fluid, central serous retinopathy manifests as an abrupt, painless vision loss.
4. Central serous retinopathy: Due to macular subretinal fluid, central serous retinopathy manifests as an abrupt, painless vision loss.
 5. Angle-closure glaucoma: The patient has a painful acute visual loss. Symptoms are red eyes with an enlarged, nonreactive pupil. treatment is iv. mannitol or oral glycerol, antiglaucoma drops and another eye preventive PI.
5. Angle-closure glaucoma: The patient has a painful acute visual loss. Symptoms are red eyes with an enlarged, nonreactive pupil. treatment is iv. mannitol or oral glycerol, antiglaucoma drops and another eye preventive PI.

6. Optic neuritis: It has symptoms of retro-orbital pain, particularly with eye movements and visual loss. Perimetry testing will most often reveal either a central scotoma or diffuse field loss. Patients have mild optic disc swelling, and retrobulbar inflammation and the optic nerve head will appear normal. MRI confirms the diagnosis. The prognosis of vision is generally good with mild residual visual dysfunction common and may be captured by measures such as contrast sensitivity and stereo acuity. The course of intravenous methylprednisolone 30 mg/kg/day for 3–5 days followed by oral prednisolone at 1 mg/kg/day with slow wean over 4–6 weeks should be given.
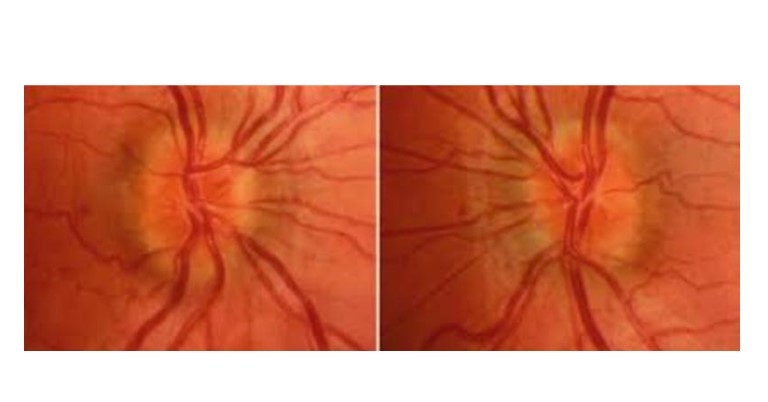
7. Papilloedema
The disc swelling in papilledema is the result of axoplasmic flow stasis in the vicinity of the optic disc. If there is an increase in cerebrospinal fluid (CSF) pressure due to any cause, the pressure is transmitted to the optic nerve causing stasis of flow.
The symptom most commonly reported was a headache. Other symptoms include visual changes (blurred vision, transient visual obscurations, double vision). The abnormal ocular motility – a false localising sign in this patient – is a result of elevated intracranial pressure.
This causes the appearance of haemorrhages and vessel anomalies at the disc This causes mechanical compression of the abducens nerve as it enters the midbrain, resulting in an abduction deficit on that side.
Therefore immediate investigations include CT scans and MRIs. Acetazolamide is a carbonic anhydrase inhibitor useful in reducing CSF production. differential diagnoses for papilledema in an otherwise healthy individual is:
- Space-occupying lesion (benign or malignant
- Idiopathic intracranial hypertension (IIH)
- Dural venous sinus thrombosis
- Typical optic neuritis
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr Jui Gharekhan (DOMS Ophthalmologist gold medalist), practices at Dr ND Desai Medical College, Nadiad, Gujarat.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries