Krait Bite Presenting as Sudden Abdominal Pain: A Case Study by Dr Ashima Sharma
M3 India Newsdesk Dec 19, 2022
Abdominal and neurological symptoms can develop simultaneously with several illnesses and inflammatory, genetic, and metabolic problems. Dr Ashima describes her experience with a case of sudden abdominal pain in this article.
The case
A 40-year-old female was brought to the emergency department with a sudden onset of severe abdominal pain, which she experienced after waking up from her sleep. The pain was colicky and was diffusely present all over the abdomen.
History
- No comorbid illnesses previously
- Was asymptomatic eight hours before the time of presentation to the Emergency Department
- She had consumed home-cooked food for dinner (freshly prepared) last night
- No history of inflammatory bowel disease, acute constipation, vomiting, dysuria, haematuria, missed periods and previous abdominal surgeries
Observations
On examination, she was conscious and oriented to time, place and person. Her pulse rate was 112/min normal sinus rhythm and blood pressure was 96/60 mmHg. Her saturations were 96% on room air; the pain score was 7/10. 18 Gauge IV cannula was kept on the dorsum of the right hand and blood samples were collected for venous blood gas, complete blood picture, serum transaminases and amylase, blood urea and creatinine and coagulation profile. She was given Inj Tramadol HCl 100 mg in 100 ml saline as an infusion over 30 min for pain relief. There were no bruises or lacerations on the abdominal wall.
The bowel sounds were hypoactive and ileus was suspected. The tenderness was diffusely spread all over the abdomen with no guarding, rigidity or rebound tenderness. The venous blood gas sample showed PCO2 of 48 mmHg, pH was 7.38 and the lactates were 2.3.
Differential diagnosis of ectopic pregnancy, appendicitis, renal colic and pancreatitis was kept. A bolus of 500 ml of saline was also given slowly to balance the third space loss. POCUS was done which ruled out intra-abdominal pathology, no fluid collections, normal kidney echotexture and normal left ventricular function.
Tachycardia was there and TAPSE(Tricuspid Annular Plane Systolic Excursion) was 2.2 cm. The chambers were not dilated and no clot or vegetation was seen. Overall, we had a patient with sudden onset abdominal pain with inconclusive examination findings. We planned to wait for the blood reports and also ordered transvaginal sonography. An orogastric tube and foley catheter was kept.
We received a call from a nurse about 45 minutes later that the patient had developed ptosis and over the next 15 mins, the patient developed severe SOB. She was gasping and was intubated with RSI using Inj Etomidate 0.6 mg/kg and Suxamethonium 2.0 mg/kg with 7.5 sizes cuffed oral endotracheal tube.
The mechanical ventilator settings were kept at full support Synchronized Intermittent volume control ventilation with FiO2 of 1.0, RR of 16, PEEP of 5 and a tidal volume of 6ml/kg (350ml). We sent an arterial blood gas sample which showed a pco2 of 26 with a pH of 7.48.
Various infections and inflammatory, hereditary and metabolic disorders can have abdominal and neurological manifestations occurring simultaneously. However, the present case when probed a little further into history revealed that the patient lives on the outskirts of the city and it is common to sight snakes in the nearby locality.
There were no fang marks on her body. It was assumed that it can still be a krait bite as it is known that signature bite marks are absent with krait bite.
Management
Without wasting time, she was initiated on WHO recommended Antisnake venom protocol by infusing 10 vials of ASV stat and 5 vials every six hours. It took four days for the patient to recover adequate muscle power for a spontaneous breathing trial.
She was extubated on Day 5 of the presentation to the hospital. Apart from ASV, Nitroglycerin infusion was required to control the sudden surges of blood pressure.
Discussion
Though uncommon, snake bite is an important differential of pain, especially in the epigastrium. It is known to occur secondary to submucosal bleeding in the stomach. Krait envenomation is the most common snake for causation. The other common clinical manifestations are depressed sensorium, hearing and vision abnormalities, paresthesias at the site of the bite, fluctuation of sympathetic-parasympathetic activity (sweating, tearing, chemosis and autonomic instability), hypokalemia, delayed neuropathy and antegrade memory loss.
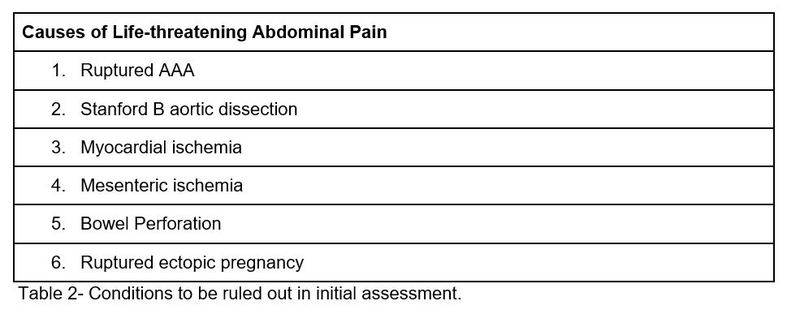
Pain abdomen has various etiologies, which can be understood based on the exact localization (Figure 2), onset (acute versus gradual), associated symptoms and signs ( radiation, quality, relieving and aggravating factors- detailed in Table 1) and Life-threatening causes (Table 2).
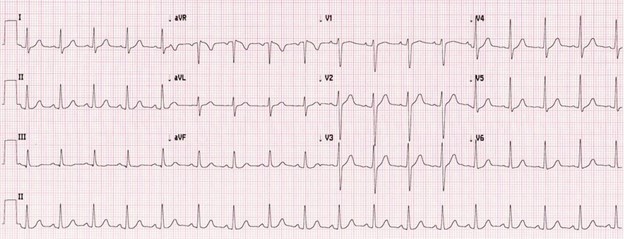
Figure 1- Sinus Tachycardia

Figure 2- Localisation of Pain for differential diagnosis
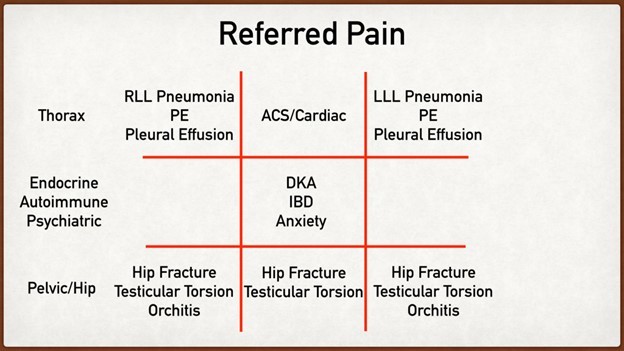
Table 1- Referred Pain for diagnosis of pathology
Take-home message
Every patient is unique and it is important to remember the uncommon causes. The use of ASV is life-saving for snake envenomation. There is no use of neostigmine and atropine is not of proven efficacy in krait envenomation.
Disclaimer- The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr Ashima Sharma is MD in Anesthesiology and critical care from Hyderabad.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries