Snakebite Management: A Comprehensive Approach
M3 India Newsdesk Jan 16, 2025
This article outlines a comprehensive care model for snakebite management, emphasising the importance of public awareness, prehospital interventions, and strengthening rural healthcare systems.
India is the World's 'Snakebite Capital' with 2.8 million bites a year with 35,000–50,000 people dying per year according to the World Health Organization (WHO) [1,2].
Lack of coordinated comprehensive care in snake bite management is the key factor behind the highest number of deaths and morbidity in India. India and our state, Assam too lacks a comprehensive care model in snake bite management.
Comprehensive care is a planned coordinated preventive, promotive, curative, mental & socioeconomic care for snake bite victims. India lacks a coordinated movement of snake bite patients from field to hospital.
Why does India need comprehensive care?
- Lack of awareness amongst the public.
- The majority attended faith healers [3,4].
- Poorly trained health care workers (HCWs) in rural districts [5,6]. Fear of HCW to administer ASV (Anti snake Venom).
- Poor transportation system to hospital.
- Delayed ASV administration [7,8]
- No support to the victim’s family due to a huge financial burden [9], if treatment is prolonged.
- No address to mental issues following a snake bite.[10].
- It is not approached as an acute emergency.
- Myth that snake bite cases can be treated only in tertiary centres.
India has huge gaps from prehospital, point-of-source hospitals to tertiary care hospitals. We need an organised care system to effectively treat snake bite victims.
Prehospital management: Venom Response Team (VRT)
Prehospital management is greatly neglected in India due to the lack of education in our society. After the snake bite our public was completely lost and often misled. A VRT was built to assist snake bite sufferers at each gramme panchayat level, which included gramme Sevak, local organisations, and ASHA workers. They can activate, communicate HCW & can transfer victims safely to the nearest hospital. It is the need of the hour. Our model focused on educating, empowering, and training the public. These trained/educated public are called VRT.


Figure: A: Community awareness programme
A. Public awareness & education is the key
We have to take the help of 3Ps. Public, Press & Politician. Nowadays, digital platforms are the best to reach out to many within a short span of time. We have to publish our own successful stories in our own local language in various digital formats.
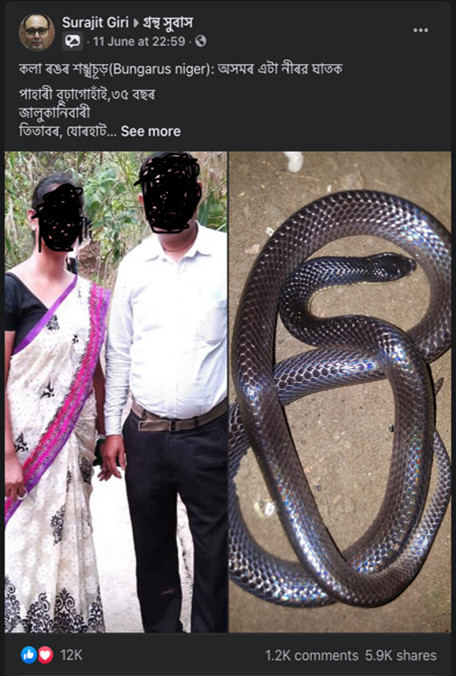


Fig1: Facebook Fig 2: TV Fig: 3 Radio
We have formed a WhatsApp group with our trained and educated general public. The name of our group is SNAKE: Public Awareness Group (Fig 4). It works like VRT. Every small community should have such a group. We are readily accessible, and we came to know about any snake bite incident in our local area, who are immediately transferred to a nearby hospital.
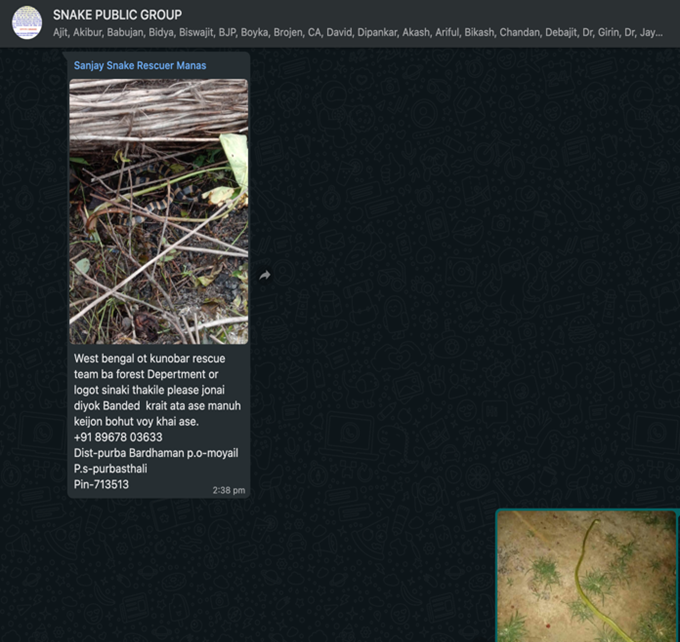

Fig 4: WA group with public Fig 5: CME with public
On 29th September 2019, we have conducted a scientific CME about snake bite with our local public and General Practitioners (Fig 5).
B. Strengthening the healthcare system
- Strengthening our rural primary (PHC) and community health Centre (CHC) is the key to a comprehensive care model. It is true that bites from Cobra, we may not get time. From 0hrs-3hrs, the patient may develop fast neurotoxic symptoms. People staying in remotest villages with envenomation symptoms, transferring such victims from CHC to district hospitals or Medical colleges without ASV administration may kill these groups of patients during transportation.
- Point of source identification (at PHC and CHC level) of venomous snake bite symptoms and administration of ASV (and neostigmine in neurotoxic) will prevent many deaths in India, which as rural CHC we have proved since year 2018. Even if patients come late to the hospital with full-blown symptoms of a PHC, our HCW should be educated and trained enough for simple manoeuvres like a bag and mask ventilation and transfer with ASV. These trained HCWs are called FRTs (Fast response teams)
- Every PHC/CHC should have a snake bite room and SOP of snake bite treatment. The snake bite room is an organised room where all medications including ASV are kept so that we can readily administer if required. Big displays (photos) of venomous snakes of the local area should be there so that patients can identify the snake that bitten him/her (Fig 6,7,8).



Fig: 6,7,8 our snake bite room in Demow CHC
C. Involving government and policymakers
Without involving the government and policy makers it is near impossible to solve the problem.
- One class/session should be included in the MBBS curriculum, especially in the 5th year (last year) of MBBS training. This class should be taken by a physician who is regularly treating snake bite victims and by a herpetologist, as there are differences in venomous snakes in different parts of India. Notably, Saw Scaled Vipers and Russel Vipers are not available in Assam except in two districts. This may be true for other states of Assam. Healthcare workers should be aware of local regional venomous snake types and their venom. If we can train/teach them at the MBBS level, the fear of handling snake bite victims will be less at the point of source (PHC/CHC level). If we start treating victims at the PHC/CHC level, many mortalities and morbidities will be prevented. We have observed that emergency departments are most of the time run by just passed Interns and as they are not trained in this subject, many a time they miss early clinical symptoms, causing unfortunate deaths. Therefore, a class/session in the last year of MBBS will greatly help them to train in the subject.
- All Government rural Hospitals should have a dedicated snake bite room adjacent to the emergency department. Recently NAPSE(National Action Plan for Snake Envenoming) has endorsed our idea of a snake bite treatment room.
- Yearly update of HCW about snake bite management.
- Referral to a higher centre should be stopped unless indicated.
- Snake bite victims should be approached as acute medical emergencies, like road traffic accidents.
- State-specific protocols should be developed depending on the venomous snakes of local and regional geographic areas.
Demow CHC comprehensive model: can be a model for India
- 400km east of Guwahati,(Capital of Assam), Demow rural CHC(Community Health Centre) started a model focusing on all components of snake bite management in the year 2018 and successfully treated 2700 numbers of victims with only one death in the year 2020.
- This rural CHC has achieved zero deaths in the year 2021(464 patients),2022(573 patients),2023(630 patients) and 2024(854 patients till 10th December).
- Demow CHC successfully formed a non-breakable chain from community to hospital. For any snake bite incident, the victim or his/her family reports to the local VRT(Venom Response Team).VRT Team will provide prehospital management. They will communicate and activate Demow Hospital. This means before the patient reaches a hospital, hospital staff are aware of the incident.
- Sometimes VRT uploads the snake photo or bitten limb on WhatsApp. They discourage tourniquets and transfer the victim with immobilisation of the limb. Within 20 minutes to 1 hr victims usually reach the hospital and are kept in the hospital for 24 hours.
- The hospital team examines the situation and uses ASV, neostigmine, and glycopyrrolate to treat early signs and symptoms at the CHC. If needed patients are transferred to a nearby tie-up ICU with bag & mask ventilation. FRT simultaneously communicates with and activates the tertiary care centre.
- Until recently, this CHC has only transferred two krait bite victims for mechanical ventilation (artificial respiration). Both are doing well. One of these two ladies was three months pregnant. As of now, both mother and womb baby are doing fine, and we are planning for the caesarian section in February 2025. Cobra and krait venom causes descending paralysis.
- This venom First attacks the cranial nerves(central nervous system nerves) and slowly progresses to the neck and respiratory muscles of the chest and diaphragm(major muscle of respiration). As in this hospital, victims attend immediately and are admitted for observation, once the neurotoxin attacks cranial nerves it causes certain symptoms like difficulty in swallowing, dysarthria(difficulty in talking), blurring of vision etc.
- This is called the golden time for healthcare workers. At this symptom, the FRT immediately infuses ASV prevents further descends of venom and ultimately prevents paralysis of respiratory muscles. If respiratory muscles are not paralysed, the definitely patient does not require any ICU or artificial respiration.
- The Demow Model VRT, FRT, Snake bite treatment room has been presented at the International Toxinology Conference, Singapore 2024, Venom and Toxin Conference, Oxford 2022 and the NAPSE 2024 (National Action Plan for Snake Envenoming) launch programme in New Delhi. NAPSE 2024 has endorsed Demow CHC's idea of a snake bite treatment room.
Results of our model
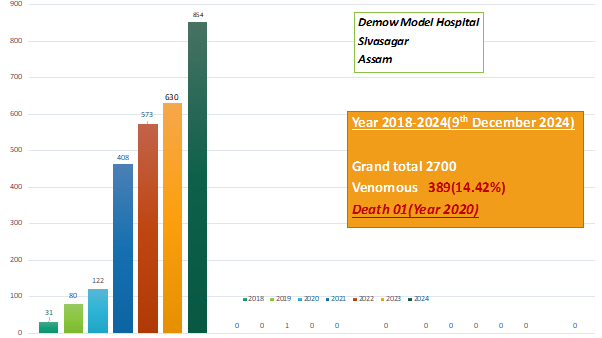
Figure: Notifications to hospitals increased tremendously due to extensive public awareness programmes.
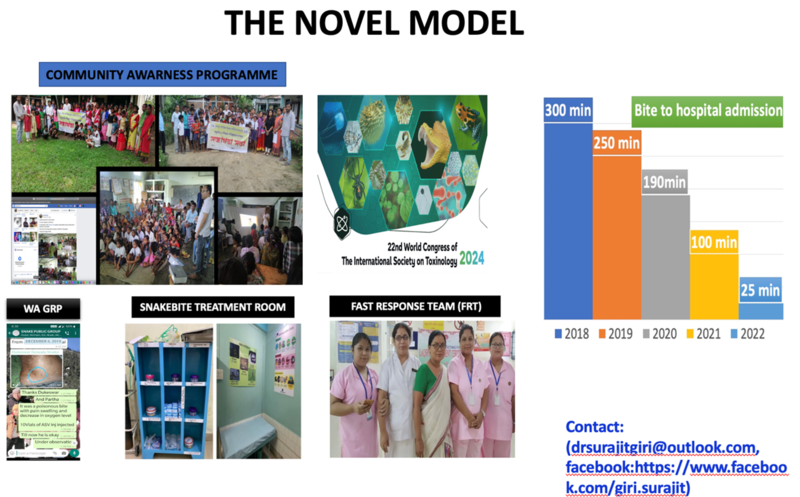
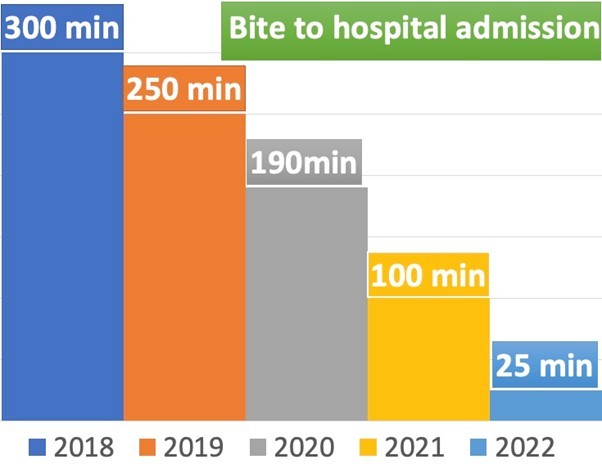
Figure: Snakebite to hospital admission time reduced to 25 minutes in the year 2022 vs 300 minutes in the year 2018.
A comprehensive model for snake bite treatment in India starts from the public, society, different social organisations, and different electronic & print media, strengthening our health care systems & manpower from the PHC level and the willingness of our policymakers and Government. We all must work as a unit, then only we can prevent many preventable deaths from snake bites. With our concept of VRT, FRT and snake bite room, we can prevent many preventable deaths as proved by our model since the year 2018.
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr Surajit Giri is Consultant Anaesthesiologist, Snake bite social activist at Demow Rural Community Health Centre, Sivasagar, Assam.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries