Russell's Viper: Deadlier than cobra! Treatment of the most lethal snake bite
M3 India Newsdesk Mar 06, 2019
One among the big four of the world's deadliest snakes and an inhabitant of ten south Asian countries this snake ranks among the most important causes of mortality.
ATTENTION: The images in this article are of snakes and patient presentations which some people may find offensive or disturbing. Viewer discretion is advised.
While protecting the paddy, wheat by containing the rodent (rats) population, Russell's viper kills many farmers unlucky enough to tread on it during harvest. It is 3 to 5 feet long. Typical rows of oval (Rudraksha) arranged in two rows is characteristic of Russell’s viper pattern. The females produce 20-60 young ones usually around June or July and the length of the fangs in adult snakes are 16 mm long and curved. The amount of venom injected at the time of bite is 63 +/-7 mg.

Viper venom
Viper venom interferes with blood clotting. It contains serine proteases, metalloproteinases, C- type lectins, disintegrins and phospholipases and exhibits both anti-coagulant and coagulant effects on blood clotting mechanism resulting in defibrination syndrome or disseminated intravascular fibrin-coagulopathy. Acute bleeding is due to hypofibrinogenaemia, due to massive consumption of fibrinogen and fibrinolysis of blood clots.
Mode of action:
- The venom, a rich source of enzymes activates factor x to convert prothrombin to thrombin in presence of calcium factor V and platelets
- Russell’s venom contains several different “pro-coagulants” which activate different steps in the clotting cascade
- The fibrinolytic activity of the viper venom is so fast that sometimes within 30 minutes of the bite, the coagulation factors are so depleted that blood does not clot
Symptoms:
- Acute renal failure due to viper bite is attributed to hypotension due to raised circulating bradykinin
- Hypovolemia due to blood loss either by external bleed or accumulation in compartments
- Severe ongoing oedema
- Smooth muscle relaxation
- Tubular blockade by free haemoglobulin, myoglobulin
- Hypo- hyperkalemia
- Tubular damage
- Interstitial nephritis
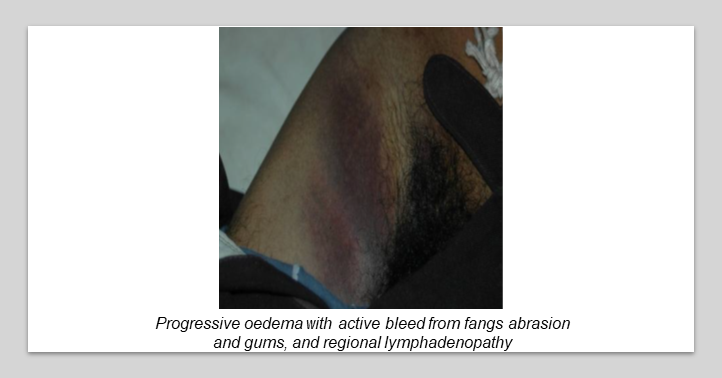
Local manifestations
Extremities are frequent targets for viper bites which occur while reaping or handling rice or Jawar or sugar cane husk bundles. The victim experiences:
- severe local pain at the site of the bite
- rapid swelling progressing to the whole limb within six to eight hours
- active bleeding from the fang marks

- no local clot formation
- local ecchymoses and tense blebs over the bitten part
- regional lymphangitis with ecchymoses within one hour
- rapid absorption of venom in circulation attributed to sharp long curve fangs injects maximum venom in deep muscles which are rich in circulation
- a rapid development of oedema muscles
- accumulation fluid and bleeding and development of compartment syndrome characterised by swelling
- painful passive movement and loss of sensation over the nerve areas passing through the compartment
- subsequent development of wet gangrene


- non-healing ulcer if left untreated results in the bitten part (usually toe or finger) to auto-amputate

Systemic manifestations
Some of the manifestations are:
- Hypotension and shock due to sudden liberation of bradykinin into circulation
- Bleeding and loss of fluid in the swollen part
- Bleeding into adrenal glands
- Pituitary or peritoneal or massive blood loss by hematemesis or hemoptysis, peritoneum, urine and skin
- Pain in the abdomen due to internal bleeding
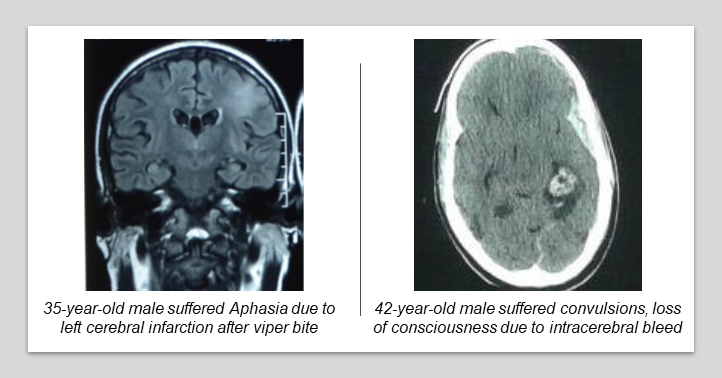
- Stroke inform of cerebral infarction due to thrombotic blockade of intracranial vessels or sub-arachnoids or intracerebral bleed or coma which may result in morbidity and mortality
- Transient recurrent ventricular tachycardia due action tumor necrosis factor content of venom which needs rapid correction by DC shock and intravenous amiodarone and ASV pro-coagulant content of venom causing rapid thrombosis, hypofibrinogenemia as result of hemostatic failure because of consumption coagulopathy
- Once the patient’s blood becomes defibrinated and incoagulable, the activity of haemorrhgins I and II damage vascular endothelium and cause platelet abnormalities which may lead to spontaneous systemic bleeding. Haematuria, bleeding in the skin and pituitary haemorrhage also occurs.
- Victims with pulmonary tuberculosis with the cavity, peptic ulcer, and hypertension are more prone to developing life-threatening bleeding. Russell’s viper bite victims subsequently develop amenorrhea, Sheehan’s syndrome, and loss of libido due to hypopituitarism (reported in a part of South India).
- Enhanced capillary permeability is seen in the form of plural, pericardial effusion, ascites, and conjunctivae haemorrhage or congestions resulting in resistant shock syndrome responsible for the high fatality.
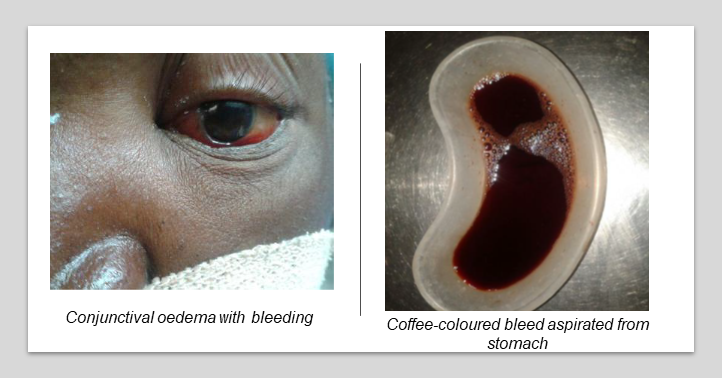
- Parotid swelling is rarely seen. Conjunctivae oedema, hypotension suggestive, oedema face, haemoconcentration, raised creatinine suggestive of leaking syndrome carries a guarded prognosis.
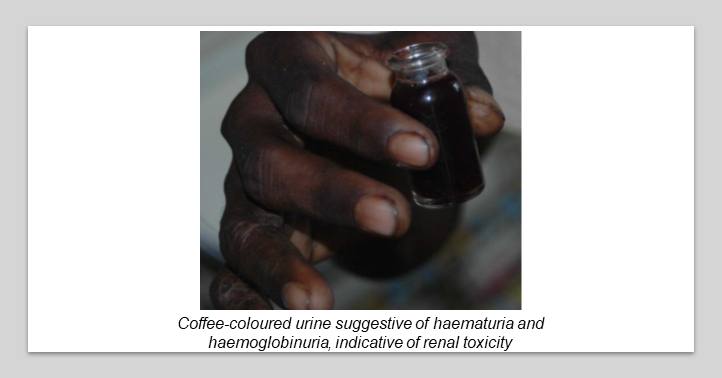
Renal failure
A common cause of fatality due to Russell’s viper bite is due to renal failure. One should keep in mind and look for renal failure from the time of admission. Risk factors such as hypotension, hypovolemia can be corrected. There are a lot of controversies regarding the early introduction of diuretic, acetyl-cysteine, or allopurinol.
However, in our experience, intravenous Lasix or torsemide 80 to 100 mg and oral acetylcysteine 600 mg, three times a day, and intravenous mannitol 100 to 200 ml may help to arrest renal damage.
20-40% cases of Russell’s viper victims subsequently develop anuria, oliguria, and acute renal failure. There is a serial rise in blood urea and serum creatinine with acidosis and hyperkalaemia. Generalised anasarca, renal failure is due to tubular damage by venom itself, haemoglobinuria, hypotension, microthrombi in the kidneys contribute to the acute tubular necrosis which is the most common cause of death.
Ptosis, bulbar palsy, inter-nuclear ophthalmoplegia and respiratory paralysis is due to a presynaptic neuromuscular block in Russell’s viper bite poisoning often seen and reported from Kerala and Sri Lanka.
Management of Russell's Viper bite victims
First-aid steps
- No attempt to apply tourniquet should be made, which may damage more local tissue
- The bitten part should be kept below heart level if active bleeding occurs
- Temporary compression may prevent massive loss of blood
Clinical protocol
- The appearance of local oedema within 30 to 60 minutes of the bite confirms snake bite with envenoming. At this time, 20 minutes whole blood clotting test (20WBCT) will be negative.

- But treatment should be started on clinical observation of local fangs marks, acute bleeding from fangs injury, and swelling. One should not wait for 20WBCT became positive.
- The bitten and swollen part should not be raised as it may cause rapid absorption of venom into the circulation.
- No intramuscular injection like tetanus should be given unless 20MWBT is done and blood clots within 20 minutes.
- 20WBCT is helpful for the second dose of ASV administration.
- Before injection of ASV, take 2 to 3 ml of blood in a new dry glass test tube which is not irrigated by any detergents
- Keep the tube undisturbed for 20 minutes and then tip it off if blood did not clot to confirm hypofibrinogenemia
- This indicates that venom is circulating in the blood and confirms the requirement for antisnake venom
Note: This test should not be done before six hours of the last dose of ASV as the liver takes six hours for the regeneration of clotting factors.
Administering ASV
- ASV- 200 ml ( 20 vials) diluted in 200 ml of 5% dextrose should be run over 30 minutes by the intravenous route
- If external bleeding does not stop within 20 to 30 minutes one can repeat with 50 ml of ASV
- The subsequent dose is to be decided by the response of 20MWBCT
- Thrombocytopenic, abnormal, cremated RBCs are a diagnosis of DIC
- In addition to ASV one has to try plasma products and whole blood transfusion which is rare but required, if ASV is administered in time with adequate dose.
- Hypotension has to be managed with fluid and inotropic agents. Severe hypotension due to bleed in adrenal and pituitary glands and abdominal bleed and endothelial dysfunction with a capillary leak may need heavy doses of intravenous methyl-prednisolone and correction of electrolytes.
Local wound care
- It is most important to avoid disability. Once the clotting mechanism is reversing (20MWBCT), the edematous limb can be elevated.
- Do a Glycerin Magsulf dressing, aspiration of tense blebs by sterile needle and debridement of dead tissues. Avoid surgical decompression unless absolutely essential.
- Surgical intervention may cause more harm than benefit. To avoid excessive bleeding before intervention by a surgeon, one should be sure that the blood is coagulable.
- Intravenous antibiotics can be given to overcome infection.
- One should always rule out diabetes mellitus.
Echis carinatus or saw-scaled viper or carpet viper
The snake is 1 to 3 feet long and is pale brown or tawny with dark brown in colour. A cruciform or trident or arrow type or just like a bird foot-print shaped mark can be seen on its head. It flourishes in hot and humid climates all over the coastal regions of India. It hibernates in the winter and often climbs on to shrubs and other low vegetation.
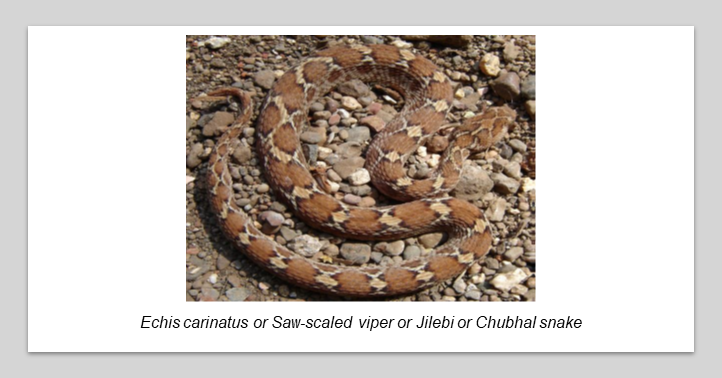
The saw-scaled viper is diurnal in habit, alert and capable of quick movement when necessary. The readiness with which it bites on the smallest provocation with extremely rapid strikes makes it is one of the most dangerous snakes. The snake is viviparous, producing 3 to 15 young ones at a time.
It injects 0.0046 g of venom at the time of the bite. Farmers, hunters, labourers, and people walking barefoot in the jungle and rocky areas often get bitten by the snake. Victims usually attribute the sudden prick caused by a viper being similar to that of a thorn prick, because it bites and runs away fast. This misinterpretation causes a delay in management at times.
- The victims develop blebs, extensive cellulite, and die of acute renal failure and septic shock. One should always keep in mind that rapid swelling with regional lymphadenitis is due to envenomation.
- A protein in the Echis carinatus (saw-scaled viper) seen all over India except Bengal and Kashmir has the unique effect of enhancing fibrinolysis by plasminogen activation by urokinase. Haemorrhagins -1, 2 and metalloendopeptidase causes acute rapid bleeding in the brain, lungs, kidney, heart and GI tract.
- It causes severe vasoconstriction followed by vasodilatation of the microvessels. Endothelial gaps due to the disintegration of endothelial cells within intracellular oedema, swollen mitochondria, dilated endoplasmic reticulum and separation of the intracellular junction of the endothelial cells. Local loss of basement membrane of the vessels leads to the capillary leaking syndrome and resistant shock.
Clinical manifestations
- Soon after the bite within one hour, there is the development of swelling over the bitten part. Fang marks or abrasions with clotted blood can be seen and swelling progress to more than one segment.
- The venom is of big molecular size and circulates through the lymphatic system. Hence, within 60 to 120 minutes the victim experiences painful lymphadenopathy at the drainage area of the bitten part.
- If untreated, swelling progresses to the whole limb or to the chest wall.
- Ecchymoses can be seen over the bitten part or may spread over the lymphatic drainage areas.
- Acute bleeding in the form of gum bleeds or bleeding from abrasions on other parts of the body or from venepuncture sites can be seen within 90 to 120 minutes of the bite.
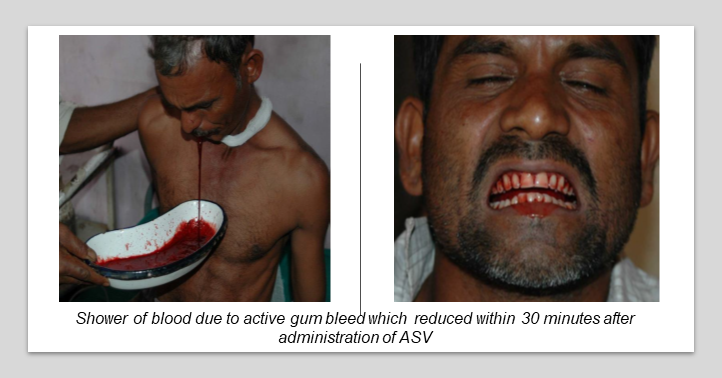
- At times, if the patient remains untreated, bleeding can persist for 1 to 2 weeks in the form of blood-stained sputum, haematuria, and disappear on its own. Such patients are markedly anaemic and report to the hospital with weakness or non-healing cellulite with uncontrolled bleeding from cellulite.
Natural immunity against Echis carinatus venom develops in case of repeated bites by the same species in endemic areas as minimum clinical involvement in such bites have been reported in Jammu region.
Renal failure due to Echis carinatus has been reported from Puducherry and Jammu areas. Management and local wound care as same as that of Russell’s viper bite. ASV requirement in Maharashtra is 30 to 50 ml. However, in Jammu and Puducherry, >100 ml may be required to correct the bleeding disorder.
Green pit viper and bamboo pit (Trimeresurus) Pit viper
Incidence is higher during monsoon season. Snakebite cases are reported from Kerala and characterised by local oedema and rarely systemic bleeding disorder. Coagulopathy and renal failure due to Hump-nosed pit viper snake bite have been reported from Kerala, which was previously thought of as a non-venomous snake.
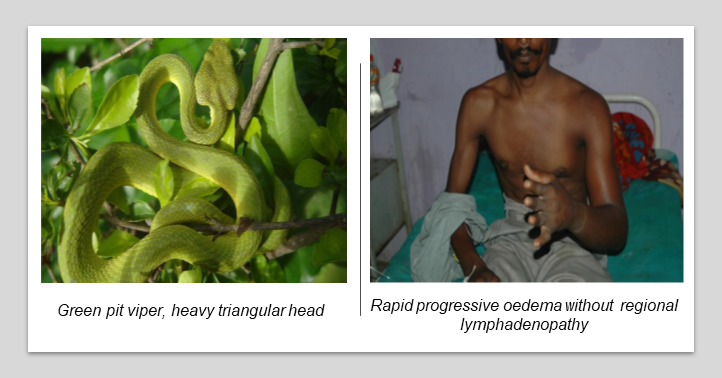
Manifestations
- The sudden rapid development of massive oedema without regional involvement.
- Rarely, the victim manifests external bleeding or renal failure.
Antivenom
No antivenom for these two vipers is available in India. However, empirical treatment with polyvalent venom could help as para specificity may sometimes help alleviate the envenoming.
- Antivenom should be administered as soon as signs of systemic or severe local swelling are seen.
- The approximate serum half-life of antivenom in envenomed victims ranges from 26 to 95 hours. Before discharge envenomed victims should be closely observed daily for minimum 3 to 4 days.
The mean times between envenoming and death are 8 hours ( 12 minutes to 120 hours) in cobras, 18 (3 to 63) hours in Bungarus caeruleus, 3 days ( 15 minutes to 264 hours) in Russell’s viper, and 5 days ( 25 to 41 days) for Echis carinatus.
Antivenom reaction and its management
- No skin test should be performed as it doesn’t give any assurance regarding reaction.
- Antivenom should not be given intramuscularly and should be administered by a qualified person having knowledge of anaphylaxis reaction and its management.

- A reaction of ASV can develop within 10 to 180 minutes.
- The incidence is increased with dose of antivenom and speed of administration.
- Bolus dose may give a rapid reaction.
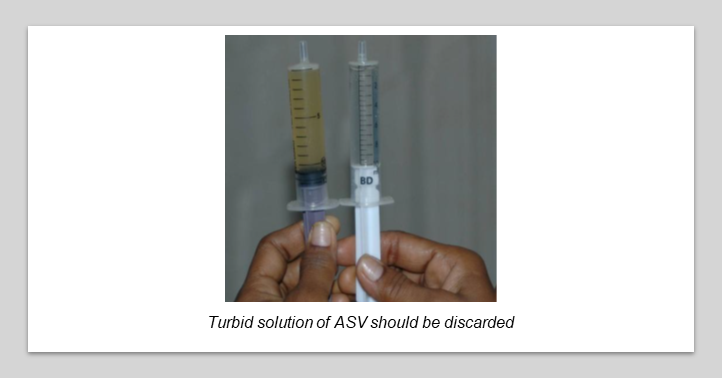
- A turbid solution of ASV may precipitate severe reaction and should be thrown away.
The earliest symptoms of a reaction are:
- hotness in ears and scalp
- itching all over the scalp
- urticaria
- sudden onset of intractable cough
- nausea and vomiting
- goose skin
- giddiness or uneasiness
- suffocation and irrelevant behaviour
- fever and tachycardia due to contamination of ASV with endotoxin-like compounds; fever, rigours, vasodilatation, and hypotension occur within 1 to 2 hours of treatment
- febrile convulsions in children
Systemic anaphylaxis
Sudden onset of projectile profound vomiting, sphincter relaxation, hypotension, bronchospasm and angio-oedema. These reactions are due to complement activation by immune complexes or aggregates of immune globulin.
Delayed reaction serum sickness can develop between 5 to 24 days of ASV therapy. Clinically characterised by pyrexia of unknown origin, itching, arthralgia, lymphadenopathy. Joint swellings, mononeuritis multiplex albuminuria and rarely encephalopathy.
Management of reaction
- Stop the ASV infusion.
- Injection adrenalin 0.5 ml of 0.1 % should be administered by intramuscular route on lateral of the thigh. The dose can be repeated if not controlled. In a situation were life is at stake such as severe hypotension, bronchospasm, or laryngeal oedema, adrenalin 1000 ug (one ml) is to be diluted in 9 cc of normal saline and total 10 cc so one ml content 100 microgram adrenalin can be given 1 ml intravenously every 5 minutes till reaction is reduced.
- In addition to this, intravenous aminophylline, intravenous normal saline, H1 blocker, chlorpheniramine maleate, intravenous methylprednisolone, and nasal oxygen may be required as well as endotracheal intubation and ventilation. Head should be at a lower position.
- Irrespective of due care, once the reaction is over and after re-administration of ASV, if the patient develops another reaction, one can select ASV from another batch and try.
- The patient should not die of reaction due to snake bite envenoming. One should not afraid of administration of ASV in a severe venomous bite provided they are fully prepared to treat the severe reaction.
- Many victims who are referred from the primary health centre to rural or district hospital without giving ASV die on the way to the hospital. Many times, we read in the referred letter that the patient is sensitive to test dose of ASV, and hence it was not administered. These are merely false excuses.
- One should sit by the side of the victim during treatment as if treating their own relatives.
Other measures
- Scientists should make attempts to prepare venomous toxoid to immunise the farmers and high-risk population against venomous snake toxins
- Toxicologists should make an attempt to prepare the pharmacological antidote to venom actions
- Antivenom producers in India should prepare Elisa kit for detection of venom antigen in blood and prepare antivenom from venoms obtained from snakes caught from relevant areas of the country
- There should be regional venom bank and antivenom preparing laboratory. The attending doctor gets immense satisfaction when the serious poor victim of snake bite recovers
The writer, Dr. Himmatrao Bawaskar is a renowned Indian physician with publications in The Lancet. He has done extensive research in scorpion sting- diagnosis and treatment protocol.
Disclaimer- The views and opinions expressed in this article are those of the author's and do not necessarily reflect the official policy or position of M3 India.
The author did not accept any payment for the article.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries