Rickets and osteomalacia in the Indian setting- Management and treatment guideline
M3 India Newsdesk May 19, 2021
Rickets and osteomalacia are often termed as twin deficiency disorder. Although both the conditions are quite similar, some fundamental differences can also be noted. This article explains the pathophysiology of calcium deficiency and the overall diagnosis and treatment protocol for the same.
An Indian perspective to the twin nutritional deficiency
Calcium deficiency is deep-rooted in the Indian population. The approach to curb the issue lies in the hands of a holistic approach. Its treatment ranges from fortification of milk to prescription of supplements to patients and awareness and education about calcium deficiency.
Introduction
Rickets results from defective mineralisation of the growth plate and is mainly seen in growing children. Osteomalacia results from defective mineralisation of the preformed osteoid and occurs both in adults and children alongside rickets. The leading causes of rickets and osteomalacia worldwide is solar vitamin D deficiency or nutritional calcium deficiency, collectively termed as nutritional rickets and osteomalacia. It has been noted that dietary calcium deficiency in isolation can also result in rickets in the absence of vitamin D deficiency or insufficiency.
Rickets can manifest the following isolated deficiency of calcium or vitamin D or following combined deficiency/ insufficiency. Calcium deficiency predominates in Asian and African continents and is mostly attributed to malnutrition and diets that are poor in calcium. Vitamin D deficiency rickets is on the rise in India due to a number of factors like:
- Lack of sunlight
- Lack of food fortification
- Ineffective supplementation programmes
- Global migration trends
Nutritional therapies
While it is relatively straightforward to increase calcium intake in the diet, there is very little vitamin D in the diet, and one relies on adequate skin synthesis following exposure to ultraviolet B (UVB) radiation in sunlight. Vitamin D synthesis in the skin can be limited due to several factors such as dark skin, high latitude residence, covered clothing, excessive use of sunscreen and sun avoidance. The latter attributes have led to the resurgence of vitamin D deficiency even in sunshine-abundant countries. However, the most vulnerable groups remain the dark-skinned immigrant and resident population of high-latitude countries, infants, and pregnant women, in particular.
Calcium and vitamin D are essential complementary nutrients for bone health. It has been noted explicitly by the National Academy of Sciences that a diet containing <50 mg calcium/100 Kcal results in osteoporosis. In the treatment of age-related bone loss and post-menopausal osteoporosis, vitamin D and calcium form an integral part of therapy. Without the mineral and Vitamin D, any anti-resorptive or anabolic agent will not have the desired effect of increasing the bone mineral density. The secondary hyperparathyroidism, an accompaniment of low dietary calcium intake (apart from maintaining normal serum calcium by leaching the bone), is also associated with high intracellular calcium ion concentrations.
Stages of hypovitaminosis D osteopathy
Rickets (or osteomalacia) is the index disease for vitamin D. Parfitt defined 3 stages of “hypovitaminosis D osteopathy” as:
Stage 1: Calcium malabsorption without histological changes (results in osteoporosis)
Stage 2: Calcium malabsorption (osteoporosis) with wide osteoid seams (early osteomalacia) without clinical laboratory features indicative of osteomalacia
Stage 3: Severe vitamin D depletion with both clinical and histological rickets or osteomalacia. Hence, mild to moderate vitamin D deficiency is expressed solely as osteoporosis, not rickets or osteomalacia. Nutritional rickets can have devastating health consequences beyond bony deformities (swollen wrist and ankle joints, rachitic rosary, soft skull, stunting and bowing) and include life-threatening hypocalcemic complications of seizures and, in infancy, heart failure due to dilated cardiomyopathy.
Diagnosing rickets
Diagnosis of rickets (always associated with osteomalacia) in children is confirmed on radiographs (cupping and flaring of metaphyses) and should be suspected in high-risk individuals with the above clinical manifestations in the presence of abnormal blood biochemistry (high alkaline phosphatase and parathyroid hormone, low 25-hydroxyvitamin D and calcium and/or low phosphate). In adults or adolescents with closed growth plates, osteomalacia presents with non-specific symptoms (fatigue, malaise and muscle weakness) and abnormal blood biochemistry, but only in extreme cases, it is associated with radiographic findings of Looser's zone fractures. Bone biopsies could confirm osteomalacia at earlier disease stages, for definitive diagnosis.
In the background of unsatisfactory levels of the combination of twin nutrient deficiency of calcium and vitamin D in India, any public health measure to address the issue in isolation may not yield the desired positive benefits for skeletal health. This problem requires to be addressed at various segments to realise the benefits, as soon as possible, by utilising the available natural resources and fortification of food. Both urban and rural population across India have to be reached.
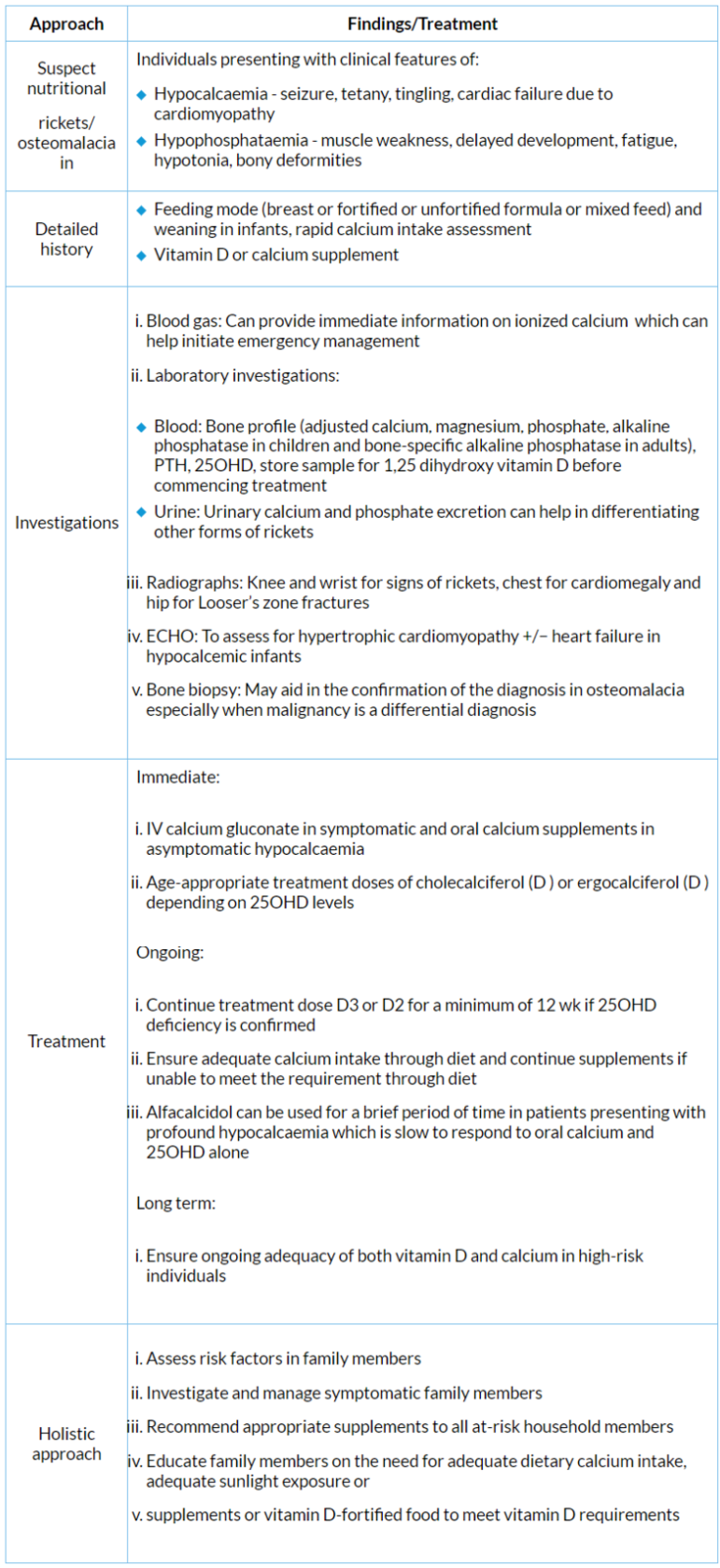
Global consensus recommendations the prevention and management of nutritional rickets
Conclusion
There is widespread dietary calcium and vitamin D deficiency in India. For over half a century, the intake of dietary calcium, milk, milk products, and cereals has declined drastically. There is a clear rural-urban divide in the consumption of dietary calcium. The deficiency of these nutrients manifests as rickets/osteomalacia and/or osteopenia/osteoporosis, which is realised at a much later age. The need of the hour is to curb the issue from the root level. Government bodies and the healthcare sector have to work alongside to achieve the goal.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries
