Renal Function Tests: All You Need To Know
M3 India Newsdesk May 11, 2023
Renal function tests are routinely carried out across all healthcare settings, with a variety of tests that can be recommended. This article provides an overview of all the necessary tests and also assists in interpreting the test outcomes.
What are the normal kidney functions?
The kidneys play a vital role in the following processes;
- Excretion of waste products and toxins such as urea, creatinine and uric acid.
- Regulation of extracellular fluid volume, serum osmolality, acid-base balance and electrolyte concentrations.
- Regulation of calcium, phosphorus and parathyroid hormone.
- Production of hormones like erythropoietin, 1, 25 dihydroxy vitamin D and renin.
Why test renal function?
- Patients with kidney disease have few signs and symptoms early in the disease course; laboratory evaluation may be the only way of detecting disease.
- Important for measuring renal disease progression and the efficacy of therapies.
- Help predict when renal replacement therapy may be necessary.
- Aid in appropriate dosing of medications.
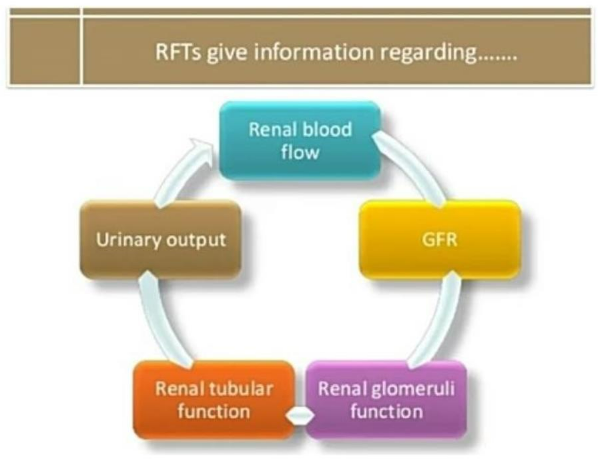
Assessment of renal function
- There are several clinical laboratory tests that are useful in investigating and evaluating kidney function.
- Clinically, the most practical tests to assess renal function are to get an estimate of the GFR and to check for proteinuria.
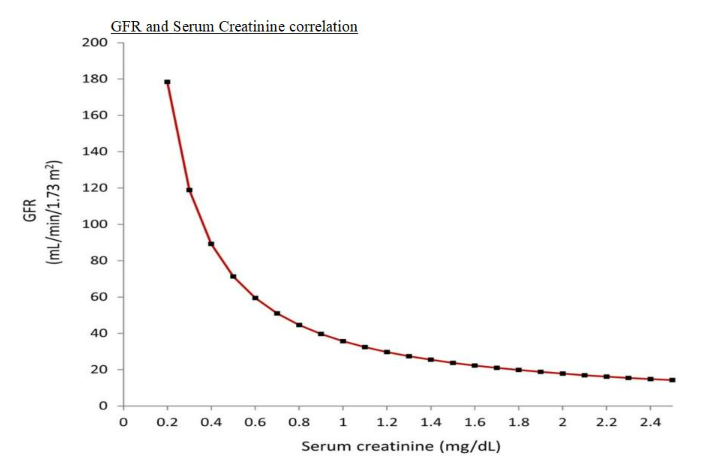
Assessment of GFR
- The best overall indicator of the glomerular function is the GFR.
- GFR is the rate in ml per minute at which substances in plasma are filtered through the glomerulus.
- The normal GFR for an adult male is 90 to 120 mL per minute.
GFR assessment
- Exogenous markers
- Inulin clearance: Gold Standard, expensive not widely available
- Radioisotopes: 125I-iothalamate, 51Cr-EDTA; accurate but expensive
- Endogenous markers
- Creatinine: Most frequently used
- Urea: Poor measure of GFR
- Cystatin C
1. Serum creatinine
- MW: 113 D
- Generated in muscles by non-enzymatic conversion of creatine and phosphocreatine and is proportional to muscle mass and relatively constant.
- The most used endogenous marker for the assessment of glomerular function.
- The calculated clearance of creatinine is used to provide an indicator of GFR.
- The National Kidney Foundation recommends the use of the CKD-EPI creatinine equation (2021) to estimate GFR.
Factors affecting serum creatinine
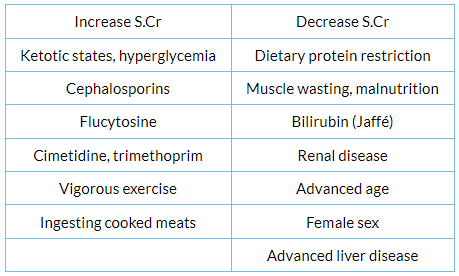
Causes of GFR variation:
- Body size: GFR conventionally factored by 1.73 m2
- Sex: GFR is approximately 8% higher in males
- Race
- Age: Age-related decline in GFR, 0.75 to 1.0 mL/min/1.73 m2 per year
- Pregnancy: GFR elevated as much as 50% in the first trimester and onward; returns toward normal by 4 to 8 weeks postpartum
- Protein intake: GFR is higher in patients on a high-protein diet
- Diurnal variation: Values tend to be about 10% higher in the afternoon than at night
- Antihypertensive therapy: Secondary to lowering of blood pressure; variable effect
2. Urea
- MW: 60 D
- One of the first indicators used to measure GFR
- Shares few features of the ideal marker and is a poor measure of GFR.
- Freely filtered but reabsorbed in proximal and distal nephron (urea clearance is less than GFR)
- Urea reabsorption is substantial in states of decreased renal perfusion.
- Urea production is variable and largely dependent on protein intake.
- State of diuresis affects urea clearance more than Ccr and is useful in the differential diagnosis of acute renal failure (ARF) where blood urea nitrogen–creatinine ratio is increased when causes are prerenal.
Factors affecting serum urea nitrogen
- Increase serum urea
- Dehydration
- Reduced renal perfusion
- Heart failure
- Increased dietary protein
- Catabolic states:
- Fever
- Trauma
- GI bleeding iv. Tetracyclines
- Corticosteroids
3. Cystatin C
- MW: 13,000 d
- Produced by all nucleated cells at a constant rate.
- Freely filtered and then absorbed and catabolised by renal tubules.
- No significant urinary excretion.
- Normal adult values range from 0.54 to 1.55 mg/dL.
- Most but not all studies show that serum cystatin C is a better index of GFR than SCr alone.
- Factors that affect the serum level of cystatin and that are independent of GFR are still controversial and possibly include older age, male sex, smoking, higher weight, thyroid disease, and higher levels of C-reactive protein.
- Additional studies across diverse populations to determine value as an index of renal function, are still required.
- It is not affected by age, muscle bulk, or diet.
- It is a more reliable marker of GFR than creatinine, particularly in early renal impairment.
- Cystatin C has also been incorporated into eGFR equations, such as the combined creatinine-cystatin KDIGO CKD-EPI equation.
Uric acid
- In humans, uric acid is the major product of the catabolism of the purine nucleosides, adenosine and guanosine.
- In humans, approximately 75% of uric acid excreted is lost in the urine; most of the remainder is secreted into the GIT.
- Hyperuricemia is defined by serum or plasma uric acid concentrations.
- > 7.0 mg/dl (0.42mmol/L) in men or > 6.0 mg/dl (0.36mmol/L) in women.
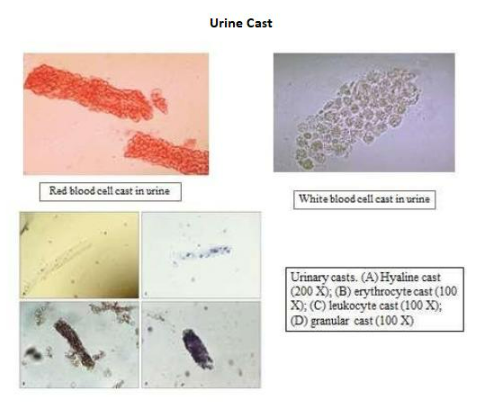
Urine examination
- Physical characteristics: Color, turbidity, odour, specific gravity
- Chemical characteristics; Ph, Hb, glucose, protein, leucocyte esterase, nitrites, ketones
- Microscopy:
- Cells: Erythrocytes, leucocytes, renal tubular epithelial cells
- Casts and crystals
Urine protein
- Microalbuminuria is now considered an obsolete term as there is no such biochemical molecule and is now referred to only as urine albumin.
- Albuminuria is used as a marker for the detection of incipient nephropathy in diabetics.
- The presence of albuminuria on two occasions with the exclusion of a urinary tract infection indicates glomerular dysfunction.
- Normal urine protein is up to 150 mg per day (30% albumin; 30% globulins; 40% Tamm Horsfall protein).

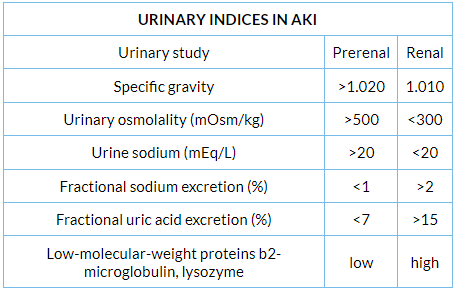
Assessment of tubular function
- Urinary specific gravity
- Urinary osmolality
- Renal concentrating capacity: Water deprivation test
- Renal diluting capacity: Water load test
- Urinary acidification: Urinary Ph, urinary anionic gap, urinary osmolar gap
- Urinary electrolytes
Other relevant kidney tests:
- Serum electrolytes
- Calcium, phosphorous
- PTH
- Vitamin D
- Iron studies
- Imaging
- Immunological workup, viral markers
- Renal biopsy
Novel biomarkers in AKI:
- NGAL (Neutrophil gelatinase-associated lipocalin)
- Kidney injury molecule 1 (KIM-1)
- L-type fatty acid-binding protein
- FGF23
- Beta-trace protein
Normal and critical findings
- The normal GFR for an adult male is 90 to 120 ml per minute.
- The presence of a normal GFR does not exclude the presence of renal disease, which may be evidenced by the presence of albuminuria/proteinuria or imaging.
- A rapidly increasing serum creatinine is considered rapidly progressive renal failure which requires immediate nephrologist consultation.
- A GFR of less than 15 ml per minute is an end-stage renal failure which may require renal replacement therapy, e.g. dialysis.
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr Bhavin Mandowara is a practising nephrologist at Zydus Hospital, Ahmedabad.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries