Recent Updates in Mammography Guidelines: Implications for Breast Cancer Screening & Diagnosis
M3 India Newsdesk Oct 27, 2023
This article outlines breast cancer screening recommendations in India, emphasising age-specific guidelines, and advanced screening techniques. It also highlights the importance of informed choices and quality assurance in mammography.
India, opportunistic screening of interested women, on a yearly basis, from the age of 40 years, is deemed appropriate.
Annual mammography is advised till the age of 70 years. Beyond the age of 70 years, it is advised that a decision is made based on the woman’s comorbidities and life expectancy.
For those already diagnosed with breast cancer and having undergone mastectomy/breast-conserving surgery for the same, annual Screening Mammography.
For high-risk women: Women who have a known BRCA 1 or 2 mutation, those with an untested first-degree relative with breast cancer, those with 20 – 25 % risk of breast cancer by validated risk assessment models, those with a history of mantle field radiation and other genetic syndromes like Li -Fraumeni syndrome constitute the high-risk group. In these women, the American College of Radiology recommends annual screening mammography starting at 30 years of age with annual screening breast MRI starting at 25 years of age up to 30 years.
For average-risk -women: Various guidelines recommend screening from 40 -to 50 years of age to the age of 70 -75 years. This can be done every year, two-yearly or three-yearly. However, the maximum benefit of this approach is found in women between 50 and 74 years of age. But, even in the age group of 40-49 years, a significant reduction in mortality due to screening mammography has been found although the quantum of benefit is less.
As per the recommendation from the Breast Imaging Society, India, 40 years is recommended as the age for starting mammography-based screening in India. Although no dedicated population-based screening program exists in contralateral or bilateral mammography respectively is recommended.
Technique
- The standard views for mammography include mediolateral oblique (MLO) and craniocaudal (CC) views of each breast.
- Digital mammography is preferred to film-screen mammography.
- This is even more important for those aged younger than 50 years and for those with dense breast tissue. On detecting a suspicious abnormality in mammography, it is helpful to further characterise the mammographic features using magnification or spot compression views.
- Sometimes other views such as the laterally and medially extended CC views and the valley view are needed to better visualise areas of the breast that are difficult to characterise on the standard views. Lateral view helps to confirm if a lesion seen on the MLO view is truly in the upper or lower half of the breast.
- Quality assurance of the mammography unit should be done regularly with specific consideration to the radiation dose delivered and the technical adequacy of films.
New techniques
1. Tomosyntheses
- The most significant difference is the use of a moving X-ray source in tomosynthesis which moves following an arc over the breast and acquires several projections.
- Numerous images per view are obtained, each showing a slice of the breast. Tomosynthesis can be acquired as an additional imaging to the usual mammograms or it can be acquired alone.
- The radiation exposure is equal to or slightly higher, as compared to mammography, but well within the limits recommended by international radiation safety guidelines.
- Tomosynthesis is able to significantly increase cancer detection by up to 30–40 % but further validation is required before routine incorporation into practice.
2. Contrast-enhanced spectral mammography
- In this technique, two exposures of the breast within the time of one compression, each with a different X-ray energy composition are acquired.
- This is possibly available for some new mammographic units and results in a low-energy image, identical to a normal mammogram, and a high-energy image containing information about contrast agent distribution in the breast.
- The use of different energies is the reason for the denomination of spectral mammography. The use of this technique also remains investigational.
3. Radiation exposure
The radiation exposure for a mammogram is low. A study reported that undergoing repeated mammograms over a time period of 34 years (annual from age 40 to 55 years and biennial from 56 to 74 years) entails a risk of radiation-induced breast cancer equal to 1 in every 1000 women screened.
The risk of breast cancer in the female population of Western countries is nearly one in every ten women. The first risk is 100 times smaller than the second, while the reduction in breast cancer mortality thanks to early detection with screening mammography is about 40 %.
4. Overdiagnosis
Not all breast cancers diagnosed with screening are aggressive and fatal cancers.
In the absence of screening mammography, some breast cancers—estimated to be about 6.5 %, with a range from 1 % to 10 % would have remained totally free of symptoms because of the very slow growth of these types of lesions, which do not tend to advance outside the breast.
As per the Euroscreen working group for every 1,000 women screened from 50 to 69 years of age,
- 7–9 breast cancer deaths are avoided
- 4 breast cancers are overdiagnosed
- 170 women have at least one recall followed by a non-invasive assessment with a negative result
- 30 women have at least one recall followed by invasive procedures with a negative result
In practice, the probability of an individual woman’s life being saved is double that of being overdiagnosed.
5. Underdiagnosis
About 28 % of cancers can be missed especially in pre-menopausal women and in those with dense breasts. Thus, if we consider 1000 women getting a screening mammogram, if 8–10 cancers are present, 2 or 3 can be missed, mostly because they are difficult to distinguish from normal breast tissue.
6. Women with dense breasts
These women should be informed about the same and given the option of supplemental screening with preferably, an MRI or ultrasound of the breast. Recently, the FDA has made it mandatory for such information to be disclosed.
7. Diagnostic mammography
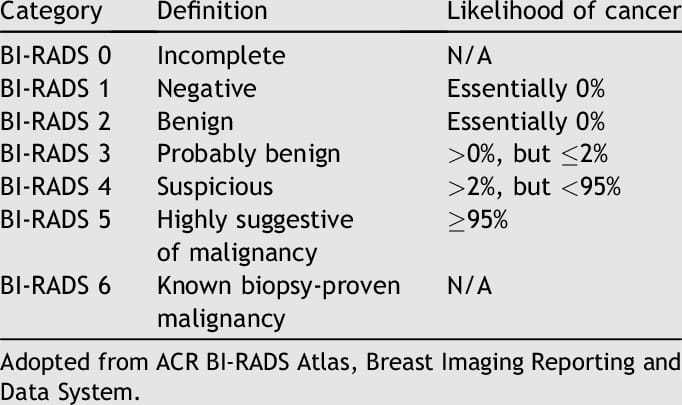
The technique remains the same and is reported as per Breast Imaging Reporting and Data System (BI-RADS) as shown in the table below.
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr Bipinesh Sansar, DM Medical Oncology, Associate Professor Medical Oncology at MPMMCC and HBCH, Varanasi.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries