Understanding Polycystic Ovarian Syndrome and its Complications
M3 India Newsdesk Oct 14, 2022
This article throws light on PCOS diagnosis, complications associated with it and its management as per the latest guidelines.
Definition
PCOS is defined as a heterogeneous clinical syndrome characterised by hyperandrogenism, mainly of ovarian origin, menstrual irregularity and hyperinsulinemia, ruling out other causes of hyperandrogenism.
Diagnostic criteria
Different endocrine societies follow b criteria to diagnose PCOS.
Rotterdam criteria (2003): At least two out of three of the following:
- Oligomenorrhea/ Amenorrhea
- Hyperandrogenism (clinical and biochemical)
- Polycystic ovaries in the US and exclusion of other disorders
Androgen excess and PCOS society (2009) criteria: PCOS is diagnosed with hyperandrogenism along with either oligomenorrhea or polycystic ovaries.
National Institute of Health Criteria 1990: The presence of hyperandrogenism and Oligomenorrhea is enough to diagnose PCOS.
Associated morbidity
Associated morbidity should be evaluated such as:
- Cutaneous manifestation: Documentation of hirsutism, skin tags, acne and acanthosis nigricans alopecia.
- Infertility: Other causes must be excluded before attributing it to PCOS.
- Obesity: Screening with help of BMI calculation and waist circumference measurement.
- Type 2 Diabetes mellitus: Fasting blood sugar to be followed by OGTT in case of a family history of diabetes. Pregnant females should be screened for gestational diabetes.
- Depression
- Endometrial cancer
- Cardiovascular risk
Investigations:
- Testosterone concentration: Often normal in PCOS patients, should be done to screen for the presence of other causes of hyperandrogenism. Levels > 5mu/l should be further investigated to rule out androgen-secreting tumours.
- LH concentration: Higher levels are associated with anovulation and infertility, it’s not a useful indicator to diagnose PCOS.
- Sex hormone binding globulin (SHBG): Low in 50 % of the patients because of hyperinsulinemia state.
- Anti- Mullerian Hormone (AMH): AMH is raised in PCOS.
Pelvis US of ovaries and endometrium: although the presence of ovarian cyst on USG is not a prerequisite for the diagnosis. The following characters seen on USG can help in diagnosis.
- 12 or more follicles measuring 2-9mm, increased ovarian size >10cc.
- Peripheral follicles may have a string of pearl appearance.
- Hypoechoic ovary without individual cyst (seen in 25 % of the patients).
For ruling out associated endocrinopathies, these tests can be performed:
- Serum prolactin.
- 17OH progesterone to exlate-onset onset congenital adrenal hyperplasia, in patients with virilization or excess testosterone >5nmol/l.
- DHEAS and androstenedione concentration: both can be raised in PCOS.
- Urinary free cortisol or overnight Dexamethasone suppression test to rule out Cushing’s syndrome.
- Thyroid profile.
Complication in PCOS
The main complications arising from PCOS can be divided into early and long-term complications. It can be categorized into Obstetrics, cardiometabolic, oncology and psychological complications. There is no clear clarification on whether the acute or chronic complications are exclusively due to PCOS or due to other existing co-morbidities like obesity.
Early-term complications are infertility and obstetrics complications
1. Infertility: In a large population of women affected by PCOS, primary infertility was reported in 50% of women, while secondary infertility was reported in 25% of women. The most recent guidelines of the Endocrine Society suggested that PCOS is a risk factor for infertility only in the presence of oligoanovulation; thus they recommended screening ovulatory status using menstrual history in all women with PCOS seeking fertility.
2. Obstetrics complications: There is an increased incidence of pregnancy complications:
- Pregnancy-induced Hypertension (12.7%) or pre-eclampsia (8%) were found to be increased by three folds.
- Gestational Diabetes Mellitus (6-15%) absolute risk is increased by three folds.
- The increase in preterm delivery is increased by two folds.
- NICU admission is increased by two folds with associated neonate mortality increasing by three times.
To avoid such complications guidelines recommend pre-conceptual assessment of BMI, BP and glucose monitoring.
Long-term complications include
1. Cardiovascular disease risk:
- Hypertension risk increases by two folds in women with PCOS.
- Dyslipidemia is very common in PCOS with a picture of increased triglyceride, decrease HDL, and decrease LDL.
- Type 2 Diabetes mellitus likeliness in a female with PCOS is three to four times.
- Lifelong metabolic dysfunction of PCOS is responsible for a worse CV profile and predisposes to cardiovascular diseases with ageing. Uncertainty still exists as to whether PCOS per se increase CV mortality.
2. Metabolic risk: There is a higher prevalence of overweight (BMI> 25) and obesity (BMI>30) in a woman with PCOS. Overall visceral obesity risk increases in such patients.
3. Oncology risk: There is an increased risk of endometrial, ovarian and breast cancer. Although there are no recommendations for routine screening or clinical cases to detect endometrial or breast cancer in women with PCOS.
4. Psychological and decreased quality of life is one of the common long-term complications seen. Depression is the most common of them which effect ranging from 14% to 67% and increasing to four folds seen in women with PCOS. Generalized anxiety is also seen in such patients.
Management
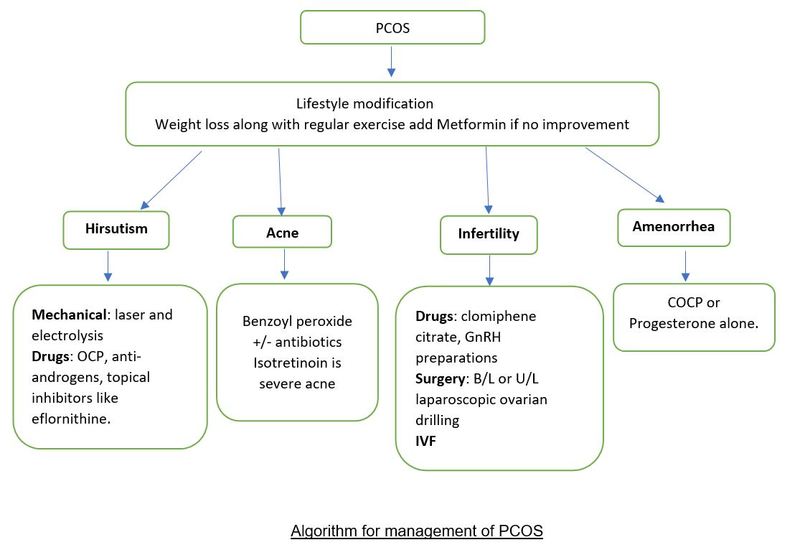
The mainstay of treatment is lifestyle modification, insulin sensitizers like metformin, pharmacotherapy for hirsutism, acne, and infertility and if medical therapy fails surgical therapy is to be considered for infertility.
1. Weight loss: It has been associated with improvement in insulin sensitivity and reduces hyperandrogenaemia. Weight loss of 5% has been associated with improvement in symptoms.
Metformin (1g-2.5g) helps in improving insulin sensitivity, with a reduction in serum androgen concentration, LH levels and improvement in SHBG levels. Metformin is used along with clomiphene citrate to induce ovulation in the patient desiring pregnancy.
2. Hirsutism: The main goal of treatment is to slow down the growth of new hair. It can be achieved by pharmacotherapy alone or along with mechanical methods of hair removal like laser therapy and electrolysis.
- Ovarian androgen suppression: Combined oral contraceptive pills or GnRH analogue.
- Androgen receptor antagonists: all are contraindicated in pregnancy.
- Spironolactone (100-200mg/day): Choice of the drug in overweight females.
- Cyproterone citrate (25-100mg) days 1-10 of pill cycle in combination with COCP
- Flutamide (125-250mg/day)
- 5 alpha Reductase inhibitors like Finasteride (1-2.5mg/day)
- Topical inhibitors of hair follicle growth: Eflornithine (11.5%)
3. Acne: The treatment should be started earlier to prevent scarring. All treatment except benzoyl peroxide is contraindicated in pregnancy.
- Mild to moderate acne: Benzoyl peroxide 5%, if no improvement after 2 months oral antibiotics are to be started.
- Moderate to severe acne: Topical retinoids like tretinoin, isotretinoin
- Oral Antibiotics: Doxycycline 100mg and minocycline 100mg/day can be continued for 3-6 months.
4. Amenorrhea: COCP, cyclical progestogen to minimize endometrial hyperplasia and metformin (up to 1gm bd).
5. Infertility
- Clomiphene citrate (25-150 mg/day) is given from day 2 of the menstrual cycle for 5 days.
- Metformin: Can be accompanied for better results along with clomiphene.
- Gonadotropin preparation: Used in patients not responding to clomiphene. Started with a low dose of 75IU/day for 2 weeks, and the dose may be increased as per response.
- Surgery: laparoscopic ovarian diathermy or laser drilling can help in restoring ovulation in 90% of the patients.
- In vitro Fertilization: When a patient fails to respond to ovulation induction.
6. Oncological Risk
In an anovulatory PCOS women who are at oncological risk should have periodic progestogen withdrawal (at least four episodes per year).
Key recommendations as per the European Endocrine Society for patients diagnosed with PCOS are as follows:
- Patients are to be screened for type 2 diabetes mellitus, hypertension and dyslipidaemia, thyroid disease, NCCAH and hyperprolactinemia.
- Weight reduction with a calorie-restricted diet in overweight patients has been associated with a positive effect on fertility and metabolic profile.
- COCP should be the choice of treatment for menstrual cycle irregularity, hirsutism, and acne in patients not planning to conceive.
Glossary
- NCCAH: Non-classical congenital adrenal hyperplasia
- PCOS: Polycystic ovarian syndrome
- COCP: Combined oral contraceptive pills
- LH: Luteinizing hormone
- US: Ultrasound
- OGTT: Oral glucose tolerance test
- GnRH: Gonadotropin-Releasing Hormone
- DHEAS: Dehydroepiandrostenedione sulphate
- BMI: Body mass index
- SHBG: Sex hormone binding globulin
Disclaimer- The views and opinions expressed in this article are those of the author's and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr Hitesh Saraogi MD, SCE Endocrinology and Diabetes(RCP, UK) is a practising physician from New Delhi.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries