Pharyngitis: What are the warning signs
M3 India Newsdesk Feb 25, 2022
Timely intervention along with an understanding of the medical history of the patient can help a clinician diagnose and treat the viral upper respiratory tract infection- Pharyngitis. This article throws light on the indicators of pharyngitis and its therapy options.
Presentation of pharyngitis
Pharyngitis is a viral upper respiratory tract infection that goes away on its own (URTIs). However, some less common causes of a sore throat must be ruled out, like COVID-19.
If you think the patient has COVID-19, ask them to get a test and follow government advice about self-isolation. This information is very important to know about the patient. It is also essential to know why the patient has come in now, and what they think, worry about and expect from you.
This could be a good time to talk to your patient about why antibiotics aren't always necessary for self-limiting viral illnesses and to do some health promotion, like giving them advice on quitting smoking.
Indicators of a troublesome condition
- Difficulty in deglutition
- Persistent sore throat for >6 weeks
- Excessive drooling
- Trismus
- Persistent cough, fever, loss of taste and loss of smell
- Unilateral facial swelling
- Dyspnoea
- Persistent unilateral tonsillar enlargement
- Immunosuppressant medication, such as carbimazole
- Photophobia
- Non-blanching rash
- Neck stiffness
Medical history
Taking a detailed history is important, but it will mostly depend on how long the symptoms have been going on. There are two types of histories: Short and long.
A short history will be more focused on infective pathology, and a long history may allow you to look into more sinister causes. The questions may include:
- Have the symptoms been prevalent for a long time; have they become worse?
- Has the patient experienced any coughing, dyspnea, fever, neck stiffness, or photophobia?
- Is there any olfactory or gustatory impairment?
- Is it difficult for them to swallow or open their mouth?
- Have they examined their own throat for anything odd, such as enlarged tonsils, pus on the tonsils, or new palate lesions?
- Do you have any symptoms that are just present on one side?
- Have they ever had these symptoms before?
- Do you have a history of acid reflux?
- Is the patient using inhalers because of a history of asthma? If that's the case, do they rinse their mouth afterwards?
- Is the patient a smoker or a heavy drinker?
- Have they noticed sneezing or itchy eyes?
A drug history may be necessary to check that individuals are not using any potentially harmful drugs, such as carbimazole or immunosuppressants. Inhalers might be the source of a chronic sore throat. If you feel that a sexually transmitted illness like gonorrhoea is causing the symptoms, you should look into the sexual history. The patient's profession, for example, if they are a singer, may be important.
Examining advice for clinicians
The COVID-19 pandemic has altered recommendations for when and how throat examinations should be performed. Throat exams in children should be avoided if at all feasible, according to RCPCH guidelines. You might have your patient use their phone to snap a photo of the back of their throat. If you still need to inspect a throat after exhausting all methods, be sure you're wearing the proper PPE.
The Royal College of Paediatrics and Child Health recommendations for tonsillar inspection
- Take a combined nose and throat swab for COVID-19 for throat examination according to local health guidelines; only check the oropharynx of children if necessary.
- PPE (apron/gloves/surgical mask) with eye protection may be used to take effective measures. It might be a visor, goggles, or safety glasses. In primary care, visors should be offered.
- If tonsillitis is suspected based on clinical history, the standard of care is to avoid examining the throat unless absolutely essential.
Examining in person
- Keep a watch for any indications of respiratory distress. Is the patient experiencing trouble opening his or her mouth? Is there any drooling or a considerable obstruction of the airway?
- Keep a close eye for indications of sepsis such as hypotension, tachycardia, and pyrexia. Examine the pharynx by opening the mouth. It's also a good idea to check oxygen saturation.
- Take a look for indicators of tonsil hypertrophy. Is this bilateral or unilateral?
- Tonsillitis comes in four different degrees, which you should be aware of. Is there any kind of exudate on the tonsils?
- Check the palate for any other severe disease, such as thrush or atypical lesions, if applicable.
- Check for lymph nodes by palpating them. If you think of infectious mononucleosis, you should palpate the spleen.
There are different grades of tonsillitis
Grade 1 - Tonsils hidden within tonsil pillars
Grade 2 - Tonsils extending to the pillars
Grade 3 - Tonsils are beyond the pillars
Grade 4 - Tonsils extend to midline
Lab tests to be advised in family practice
Most cases of pharyngitis may not need further investigation, however, depending on the history, you may want to explore the following tests:
- Complete blood count (CBC) - If you suspect neutropenia or infectious mononucleosis, this test may be necessary. Make sure you have a strategy in place for dealing with the CBC outcomes. If you suspect agranulocytosis in a patient on carbimazole, for example, you may want to refer the patient to the hospital for further investigations.
- Monospot test
- Throat swab
- Helicobacter pylori faecal antigen test or serology - Helicobacter pylori faecal antigen test or serology (depending on your local policies for this).
- HIV testing may be necessary based on the patient's medical history and concerns about seroconversion.
- Gonorrhoea swab
- COVID-19 test
- Chest X-ray if persistent respiratory symptoms are present.
When should you consult an expert?
- A regular referral to an ENT for additional assessment is required if you have had an unexplained sore throat for more than 6 weeks. If red flag symptoms exist, you may want to refer after a two-week delay.
- If there is trismus, drooling, or indications of quinsy on examination, as well as symptoms indicative of meningitis, same-day admission is required.
- Admission is required if neutropenia is detected on the FBC. Persistent unilateral tonsillar growth will need a two-week wait time before being referred.
- Consult a genitourinary specialist if you feel you have gonococcal pharyngitis.
Pharyngitis causing factors
- Viral tonsillitis
- Infectious mononucleosis
- Quinsy
- Tonsillar malignancy
- Thrush
- Hayfever
- HIV seroconversion sickness
- Gastro-oesophageal reflux disease (GORD)
- Iatrogenic causes such as carbimazole
- COVID-19
- Singing may make a person more susceptible to a prolonged sore throat
- Pharyngitis related to gonococcus
Options for therapy
- Treatment choices are determined by the cause. In the absence of red flags or major examination findings, acute viral pharyngitis should be treated conservatively, with a focus on symptom management.
- A thorough explanation of why antibiotics aren't needed, a discussion of red flag symptoms, and a discussion of when symptoms should be expected to resolve should sufficient. You may want to think about getting antibiotics on hold.
- Antibiotic selection and duration should be guided by your local health board's antimicrobial policy.
- To rule out a malignant disease, persistent unilateral tonsillar hypertrophy may necessitate biopsy under the supervision of an ENT. Patients with symptoms of quinsy will need to be admitted to an emergency ENT clinic for drainage. Initiation of the GORD pathway will be required if GORD is suspected.
- Confirmed infectious mononucleosis does not need therapy beyond informing the patient about what to anticipate in terms of symptom relief and possible consequences such as splenomegaly. If applicable, it would be prudent to advise avoiding contact sports for a period of four weeks.
- Antihistamines, intranasal steroid spray, and suitable eye drops are likely to be required if hay fever is suspected.
- Speech and language therapy may be required for an occupational purpose.
- Thrush caused by steroid inhalation medication may need instruction about proper mouth care following inhaler use.
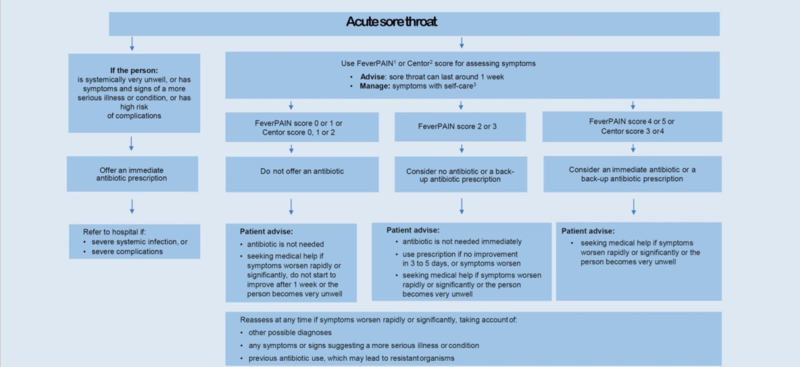
FeverPAIN score for antibiotics decision
The validity of the FeverPAIN score has been established. It considers the existence of a fever during the previous 24 hours, the absence of a cough or coryza, and the beginning of symptoms within the last 72 hours.
Tonsil infection or purulent tonsils are among the examination results. A score of 1 indicates that antibiotics are not needed, a score of 2 to 3 indicates that a prescription should be postponed, and a score of 4–5 indicates that antibiotics are required.
The FeverPain criteria are:
Score 1 point for each (maximum score of 5)
- Fever over 38°C
- Purulence(pharyngeal/tonsillar exudate)
- Attend rapidly (3 days or less)
- Severely Inflamed tonsils
- No cough or coryza
A score of 0 or 1 is associated with a 13% to 18 % likelihood of isolating streptococcus.
A score of 2 or 3 is associated with a 34% to 40 % likelihood of isolating streptococcus.
A score of 4 or 5 is associated with a 62% to 65 % likelihood of isolating streptococcus
Acute sore throat- Antimicrobial prescribing
Click here to see references
Disclaimer- The views and opinions expressed in this article are those of the author's and do not necessarily reflect the official policy or position of M3 India.
The author is a practising super specialist from New Delhi.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries