Pembrolizumab as a potential option for thymic cancer?
M3 Global Newsdesk Apr 06, 2018
A study published in Lancet Oncology reported that pembrolizumab demonstrated anti-tumor activity in patients with thymic carcinoma, although a small proportion of patients developed severe autoimmune toxicity.
The study was led by Giuseppe Giaccone, MD, PhD, from the Lombardi Comprehensive Cancer Center at Georgetown University in Washington, DC. It evaluated pembrolizumab in patients with recurrent thymic carcinoma who had progressed after chemotherapy to assess overall response (OR) as well as progression-free survival (PFS), overall survival (OS), and safety.
Thymic carcinomas are the most aggressive subtype of rare thymic epithelial tumors. They are often not resectable, tend to metastasize widely, and are associated with a shorter OS than thymomas, as response rate to standard treatment is less than 50%.
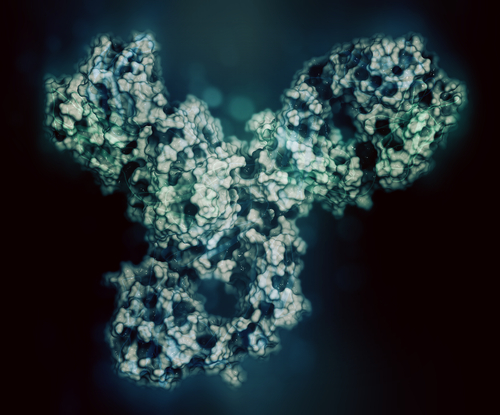
Immune checkpoint inhibitors such as pembrolizumab, a programmed death-ligand 1 (PD-L1) antibody, are effective in treating other malignancies. Since thymic carcinomas have a high expression of PD-L1, the investigators designed a study to evaluate pembrolizumab in patients with advanced refractory or recurrent thymic carcinomas.
Pembrolizumab is an active treatment in patients with advanced thymic carcinoma. The response and response duration of pembrolizumab compares favorably with other treatments that are available for this disease.
Patients with a histologic diagnosis of thymic carcinoma treated with at least one previous chemotherapy regimen were given pembrolizumab 200 mg intravenously every three weeks for up to two years; dose reductions were not allowed. Treatment was withheld in patients with grade 4 hematological toxicities and with grade 3 and above non-hematological toxicities, and it was discontinued for confirmed progression, unacceptable toxicity, or on patient request.
Physical examination, blood cell count, and urinalysis were performed before every treatment cycle, and thyroid function was evaluated every two cycles. Tumor response was assessed with CT scans every two cycles for the first year, every four cycles for the second year, and every three to four months thereafter.
Immunohistochemistry was used to determine PD-L1 expression
The primary endpoint of the study was the proportion of patients who achieved an overall response (a radiologically confirmed complete or partial response). Duration of response was assessed ad hoc from the first assessment of response to progression. Secondary endpoints were PFS, OS, and safety.
A total of 40 patients were eligible. Most were white (82%), male (70%), and had extensive metastatic disease. The median follow-up was 20 months. The overall response rate was 22.5%. One patient had a complete response and eight had partial responses. Additionally, 21 patients had stable disease and ten had progression. Disease control (complete or partial response plus stable disease) was achieved in 30 patients.
Median time to response was 6 weeks (range 6–24). The median duration of response for nine patients with a complete or partial response was 22.4 months. For 21 patients who reported stable disease, the median duration from the start of treatment was 6.8 months. Of these, stable disease was maintained for at least six months in eight patients, and for more than a year in three patients. Median PFS was 4.2 months and median OS was 24.9 months. One-year PFS was 29%, and 1-year OS was 71%.
Patients received a median of six cycles (range 1–35) of pembrolizumab treatment. The major reason for treatment discontinuation was disease progression. Most adverse events were mild and similar to those typically reported with pembrolizumab. The most common grade 3 or 4 adverse events were increased aspartate aminotransferase and alanine aminotransferase levels (five patients each). However, six patients developed one or more new-onset severe immune-related adverse events (irAEs). All recovered, and three had a partial response to therapy.
PD-L1 immunohistochemistry data were available for 37 patients. High PD-L1 expression was found in ten patients, six of whom had a partial or complete response (P=0.005). In a post-hoc analysis, PFS was longer in patients with high PD-L1 expression than in those with low or no expression (median 24 months vs 2.9 months). OS was also longer in patients with high expression than in those with low or no expression. Gene expression profiling and targeted exome sequencing was done for some patients to evaluate associations with OS or to predict patients who may be at higher risk of toxicity.
They advised that the autoimmune disorders that may result from treatment can be severe in some cases, but they are typically manageable with careful monitoring, preventive measures, frequent measurements of troponin and creatine phosphokinase, and screening for the presence of high levels of autoantibodies.
To read more about this study, click here.
This story is contributed by Robyn Boyle and is a part of our Global Content Initiative, where we feature selected stories from our Global network which we believe would be most useful and informative to our doctor members.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries