Obstructive Sleep Apnoea: Most Underdiagnosed Health Condition
M3 India Newsdesk Oct 03, 2023
This article evaluates obstructive sleep apnoea (OSA), in particular, its diagnosis, and treatment options, as well as the possible advantages of bariatric surgery in obese OSA patients.
Definition & epidemiology
Sleep-disordered breathing includes abnormal respiratory patterns (apnoea, hypopnea, or respiratory effort-related arousals) or central sleep apnoea-hypopnea syndrome including cheyne-stokes breathing syndrome or central hypoventilation leading to altered gas exchange.
- OSA and OSAS are subsets of sleep-disordered breathing.
- OSA is the occurrence of an average of 5 or more episodes of obstructive respiratory events (apnoeas, hypopneas, or areas) per hour of sleep with either sleep-related symptoms or comorbidities or ≥ 15 such episodes without any sleep-related symptoms or comorbidities. OSAS is an OSA associated with daytime symptoms, most often excessive sleepiness.
- Community-based epidemiological studies from India have shown that the prevalence of OSA is 2.4% to 5 % in males and 1 to 2% in females.
- There is no considerable variation in the majority of OSAS compared to the rest of the world where it is 4% in males and 2% in females.
Risk factors
- Older age
- Male gender
- Post-menopausal state
- Obesity
- Central body fat distribution
- Increased neck circumference
- Several anatomical abnormalities of the craniofacial region and upper airway
- Tobacco smoking
- Alcohol use
- Night-time nasal congestion
- Endocrine abnormalities (hypothyroidism, acromegaly), polycystic ovarian syndrome
- Down’s syndrome
- Drugs (benzodiazepines, muscle relaxants, testosterone therapy)
It is usually associated with several co-morbidities such as insulin resistance, diabetes mellitus, hypertension, stroke and coronary artery disease. OSA increases mortality either due to apnoea per se, increased risk of vehicular accidents or associated co-morbidities.
Diagnosis
- History and physical examination are crucial first steps towards the recognition and diagnosis of OSA.
- Patient history should focus on nocturnal breathing abnormalities, daytime sleepiness, and family and personal medical history.
- Consider using the stop-bang questionnaire to help determine if a patient is at increased risk of moderate to severe OSA.
OSA symptoms include
- Fatigue
- Habitual loud snoring
- Choking, gasping, or pauses in breathing during sleep
- Morning headache
- Recurrent night-time awakenings
- Unrefreshing or restless sleep
- Impaired concentration
- Nocturia
Physical examination
Head and neck examinations are important. Measure the neck circumference if feasible examine the upper airway and it may be useful to evaluate the Mallampati score – Mallampati classification.
A higher Mallampati classification has been associated with osa diagnosis and increased ahi. For every 1-point increase in the Mallampati score, the odds of having OSA increased by more than 2-fold.
Polysomnography
- The use of PSG for evaluating OSA requires recording the following physiologic signals: electroencephalogram (EEG), electrooculogram (EOG), chin electromyogram, airflow, oxygen saturation, respiratory effort, and electrocardiogram (ECG) or heart rate.
- Full-night PSG is recommended for the diagnosis of a sleep-related breathing disorder but a split-night study (initial diagnostic PSG followed by continuous positive airway pressure titration on the same night) is an alternative to one full night of diagnostic PSG.
- The split-night study may be performed if an ahi ≥ 40/hr is documented during 2 hours of a diagnostic study but may be considered for an ahi of 20-40/hr based on clinical judgment.
- In patients where there is a strong suspicion of OSA if other causes for symptoms have been excluded, a second diagnostic overnight PSG may be necessary to diagnose the disorder.
- The diagnosis of OSA is confirmed if the number of obstructive events (apnoeas, hypopneas + respiratory event-related arousals) on PSG is greater than 15 events/hr or greater than 5/hour.
OSA severity is defined as;
- Mild for rdi ≥ 5 and < 15,
- Moderate for rdi ≥ 15 and ≤ 30, and
- Severe for rdi > 30/hr
OSA management
1. Healthy behaviours and diet
The importance of healthy behaviours and diet, including exercise and weight loss, should be recommended for patients with elevated BMI, although it is not adequate as a stand-alone therapy if the patient is sleepy or has moderate to severe OSA.
Weight loss is more successful if the patient uses definitive therapy to control their OSA and then retests after their weight goal is achieved to see if definitive therapy is still required.
2. Continuous Positive Airway Pressure (CPAP)
CPAP is generally the most effective treatment for OSA. Auto CPAP machines, BiPAP machines and other newer machines with different modes are available for patients.
3. Positional therapy
Avoiding sleeping in the supine position is an option if testing shows that OSA is primarily in the supine position. There are electronic devices that can monitor and record sleeping positions.
4. Oral devices
- Mandibular advancement device (MAD)
Is an appliance that fits over the upper and lower teeth with an adjustment to push the lower jaw forward. The device brings the tongue forward creating a more patent airway. Although expensive, for those that it works for, a custom device can be as effective as CPAP and often better tolerated. Patients may experience jaw or dental pain from MAD's which may inhibit use. Some movement and misalignment of the teeth may occur, but usually resolves itself if treatment is discontinued within the first year of treatment. Note there are many brands of MADs. The ones using rigid bars or screws are likely to be more effective than those using elastic straps to pull the lower jaw forward.
- Tongue retaining device
Is a flexible, silicone device that fits behind the lips in front of the teeth. It is a relatively inexpensive way of controlling snoring or very mild OSA with few side effects, compliance is generally low.
“Boil and bite” devices are much less expensive but are bulky and made of a soft material that does not last as long. They are usually patient-fitted, more prone to complications and much less effective.
- Other devices
Devices such as adhesive nasal strips and nasal dilators may help nasal airflow but do not directly address the obstruction in the oral-pharyngeal airway that causes OSA.
Similarly, chin straps may keep the mouth closed but do not correct the oral-pharyngeal airway obstruction. There is also a very real danger of an improperly applied strap pushing the jaw back and causing more obstruction.
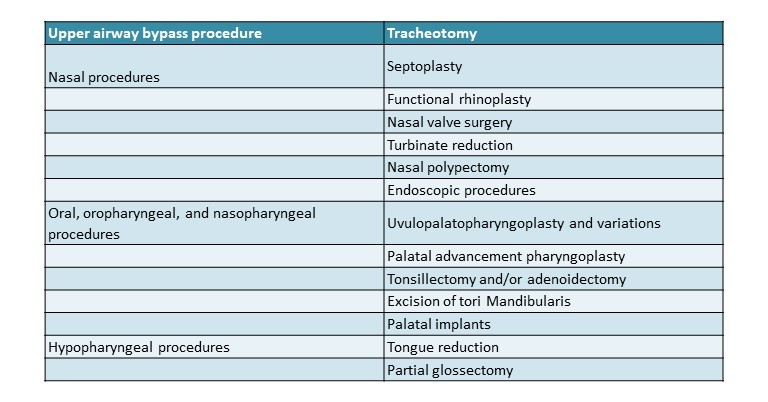
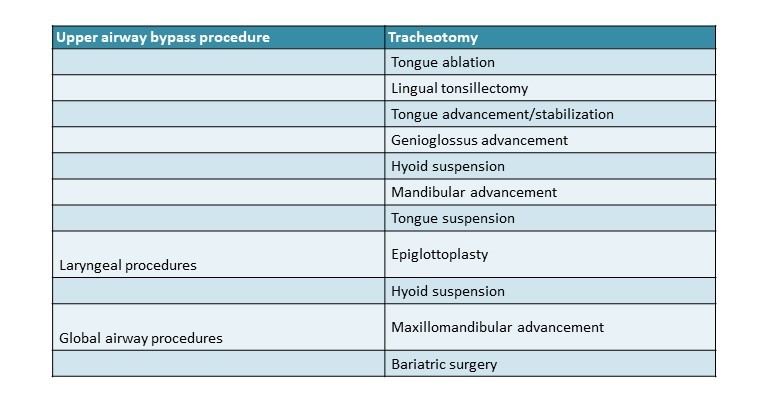
Common surgical procedures for OSA
Adjunctive therapies
Bariatric surgery
- Bariatric surgery is an effective means to achieve major weight loss and is indicated in individuals with a body mass index (BMI) ≥ 40 kg/m2 or those with a BMI≥ 35 kg/m2 with important comorbidities and in whom dietary attempts at weight control have been ineffective.
- Bariatric surgery may be adjunctive in the treatment of OSA in obese patients bariatric surgery should be considered as an adjunct to less invasive and rapidly active first-line therapies such as pap for patients who have OSA and meet the currently published guidelines for bariatric surgery.
- The remission rate for OSA two years after bariatric surgery, related to the amount of weight lost, is 40%, emphasising the need for ongoing clinical follow-up of these patients.
Pharmacologic agents and oxygen therapy
- Individuals with hypothyroidism or acromegaly. Treatment of those underlying medical conditions can improve the ahi. Specifically, selective serotonergic uptake inhibitors (SSRI) protriptyline, methylxanthine derivatives (aminophylline and theophylline) and estrogen therapy (estrogen preparations with or without progesterone) are not recommended for the treatment of OSA.
- Short-acting nasal decongestants are not recommended for the treatment of OSA but topical nasal corticosteroids may improve the ahi in patients with OSA and concurrent rhinitis, and thus may be a useful adjunct to primary therapies for OSA.
- Oxygen supplementation is not recommended as a primary treatment for OSA ( if supplemental oxygen is used as an adjunct to other primary therapies to treat hypoxemia, follow-up must include documentation of resolution of the hypoxemia supplemental oxygen alone may reduce nocturnal hypoxemia but may also prolong apnoeas and may potentially worsen nocturnal hypercapnia in patients with comorbid respiratory disease.
General OSA outcomes assessment
- Resolution of sleepiness
- Osa-specific quality-of-life measures
- Patient and spousal satisfaction
- Adherence to therapy
- Avoidance of factors worsening disease
- Obtaining an adequate amount of sleep
- Practicing proper sleep hygiene
- Weight loss for overweight/obese patients
Takeaway point
If any obese patient with a short neck comes to you with complaints of excessive daytime sleepiness and nighttime snoring and awakening with comorbidities like hypertension, DM, or dyslipidemia, then always keep OSA as a diagnosis in mind and do the necessary workup for the same. Treating OSA will significantly improve the morbidity, mortality and quality of life of patients.
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr. Nisarg Patel (UGC), MD Pulmonology, Omkar Chest Care and Medical Hospital, Ahmedabad.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries