New Treatment in Uveitis
M3 India Newsdesk Mar 07, 2025
This article delves into noninfectious uveitis, highlighting innovative treatments that minimise risks and maximise vision preservation.
Uveitis is inflammation of the Uveal tissue and can involve the iris, ciliary body, choroid or the whole uveal tissue. Uveitis can be infectious or non-infectious. Noninfectious uveitis can be due to immunological causes and is usually associated with autoimmune systemic diseases.
There is a long list of noninfectious causes of uveitis as below:
- Acute Anterior Uveitis
- RA-associated uveitis
- HLA B 27 positive Uveitis
- Sarcoidosis
- Behcet’s disease
- Systemic Lupus Erythematosus
- Multiple sclerosis
- Drug-induced
Recurrent and long-term chronic uveitis can lead to ocular complications such as:
- Blurred vision
- Glaucoma
- Synechiae formation
- Band-shaped keratopathy
- Corneal degeneration
- Complicated cataracts
- Cystoid macular edema
- Retinal vasculitis
- Retinal hemorrhage
- Retinal tear
- Retinal detachment
Delineating a precise etiology of uveitis requires a battery of investigations which determines the course and prognosis of the disease and formulation of a management strategy. In this communication, our focus is on diagnosis and novel management strategies for uveitis.
Step Ladder Approach for Management of Uveitis
- Steroids and atropine
- Immunomodulators
- Antimetabolites- Methotrexate, Mycophenolate mofetil, Azathioprine
- Calcineurin signal inhibitors in T cells- Tacrolimus, Cyclosporin A, voclosporin, Sirolimus
- Alkylating agents- Cyclophosphamide, chlorambucil
- Bio pharmacological agent ( Biologics )- Infliximab ,Adalimumab , etanercept ,golimumab, certolizumab
A systematic approach toward noninfectious uveitis patients is the initiation of topical/oral steroids and consideration of intravitreal steroids in cases of non-resolving macular oedema. Alternatives include Oral methotrexate/Mycofenolate mofetil. The second line of therapy is TNF alfa blockers/Biological agents. Commonly used agents include Infliximab and adalimumab, whereas Certolizumab and golimumab are novel drug options.
Newer biological agents include tocilizumab(IL6 inhibitor), Vamkibart (IL6 inhibitor ) and Tofacitinib (JAK 1 & 3 inhibitor ).
Steroids
The first line of therapy in any case of uveitis suppresses inflammation in acute stages ( if there are no contraindications for use). These can be used as topical, oral, sub-tenons, Orbital floor injections and in the form of intravitreal Triamcinolone and Dexamethasone Depot implant ( Ozurdex )
Immunomodulators
Immunomodulators modify the immune response/functioning of the immune system (by the stimulation of antibody formation or the inhibition of white blood cell activity). Immunomodulator therapy should be considered in the following conditions.
- Vision-threatening ocular inflammation
- Intolerable side effects owing to steroid use
- Inadequate response to corticosteroids
- Long-term dependence on steroid therapy
- Contraindications of steroid therapy
Before starting Immunomodulators patients should not have any active infection (including fungal) and live vaccines should be avoided at this point in time. These medicines are contraindicated in pregnancy. Renal, hepatic and bone marrow disease must be ruled out. Maintenance of good hygiene is important, and Patients should be regular with follow-up visits. CBC, Renal Function Tests and Liver Function Tests should be done.
A. Anti metabolites
1. Methotrexate
It is a Folic acid antagonist and inhibits Dihydro folate reductase preventing DNA and RNA formation. In addition, it increases adenosine levels which inhibits inflammation.
Indications: Inflammatory conditions like Rheumatoid arthritis, psoriasis, cancer (leukaemia), Organ transplantation, Uveitis, Scleritis and JIA.
- Adverse effects:
- Hepatotoxic
- Allergic reactions
- GI toxicity
- Chest pain
- Renal problems
Contraindicated during pregnancy, HIV, Blood dyscrasias and Radiotherapy patients and can cause megaloblastic anaemia. Vitamin B6 supplementation is required along with this.
The dose can start from 7.5 mg up to 15 -25 mg weekly orally / injectable.
2. Mycophenolate mofetil- 2-3 gm daily orally or injectable
Mechanism of action: Inhibits Purine biosynthesis and suppresses the immune system.
Indications: Chronic recurrent uveitis, posterior uveitis, Scleritis, Ocular Cicatricial Pemphigoid,
Atopic keratoconjunctivitis, Graft rejections, Thyroid eye disease and optic neuritis.
Adverse effects: GI Toxicity, colitis
As per SITE analysis (Systemic Immunosuppressive Therapy for Eye Disease) it is documented that mycophenolate mofetil acts rapidly than methotrexate but by 9 months both were equivocal. In this study, an escalation approach was used, and mycophenolate was started at 2gm daily dose and escalated up to 3 gm while methotrexate was initiated at 10 mg weekly and escalated up to 15 mg /weekly as per requirement.
3. FAST (First Line Anti Metabolites for steroid-sparing agents)
The trial compared efficacy between methotrexate and mycophenolate mofetil and concluded that both are equivocal.
4. Azathioprine
It is mainly used in Systemic lupus erythematous, myositis and Rheumatoid arthritis. It can be used in uveitis and other ocular inflammatory diseases like retinal vasculitis, sympathetic ophthalmitis, Bechet disease and prevention of graft rejection.
Doses-1 to 3 mg/kg/day PO (100-250mg QD)
Adverse effects include nausea, vomiting, and Skin rashes, hence limiting its usefulness. SITE (Systemic Immunosuppressive Therapy for Eye Disease) has illustrated that Azathioprine has a moderate success rate.
Indications: Uveitis, Behcet disease, serpiginous retinochoroiditis, sympathetic ophthalmia, Vogt kayanagi Harada disease.
B. Calcineurin Inhibitors
- Tacrolimus
Calcineurin Inhibitor via binding intracellular protein (FK 506 ) Common indications are severe dry eyes, Sjogren’s syndrome, SJS, Atopic conjunctivitis and Corneal transplant.It is available in Oral and Ointment forms
- Cyclosporine
A Blocks T Cell activity via calcineurin inhibition pathway. Indications are similar to tacrolimus but can be used in OCP also. Doses -2.5- 5mg/kg/day PO 10mg/kg/day
C. Biological agents
Biologics are bioengineered molecules produced in living systems and are used therapeutically to target cellular receptors or cytokines responsible for inflammation. Biologics are increasingly being used to treat uveitis that is unresponsive to more conventional forms of immunosuppression.
Monoclonal antibodies (mab) are biologics that act via anti-tumour necrosis factor (TNF) agents and inhibit T cell / CD4 mediated inflammatory reaction and can be of great utility to retina specialists managing chronic noninfectious uveitis refractory to steroids and first-line steroid-sparing agents. These drugs assist a retina specialist in the therapeutic armamentarium against recurrent disease and improve patient outcomes in association with rheumatologists.
1. Infliximab
Infliximab is a monoclonal human chimeric immunoglobulin G (IgG) antibody directed against TNF-α and is used in the treatment of conditions like:
- Rheumatoid arthritis
- Juvenile idiopathic arthritis (JIA)
- Crohn's disease
- Ankylosing spondylitis
- Psoriatic arthritis
- Plaque psoriasis
- Ulcerative colitis
It is administered through an intravenous route. It is indicated for use in refractory uveitis, scleritis, posterior uveitis and Behcet disease. It is usually administered in three doses of 200mg infusions spaced at two weeks.
Side effects are rare and include:
- Infection
- Reactivation of latent tuberculosis and malignancies
Precaution: Screening for infectious diseases like tuberculosis infection, hepatitis B, hepatitis C, and HIV is a must. Underlying malignancy and immuno-compromised individuals are contraindications and vaccination should not be done during the course of therapy. Demyelinating diseases, such as multiple sclerosis can also get aggravated by using these drugs.
2. Adalimumab
Adalimumab was the first human monoclonal antibody approved by the FDA. It acts by binding and neutralizing TNF-α and can be administered subcutaneously via preloaded syringes rather than intravenously. It is generally given 40 mg/0.8 mL every 2 weeks, which can be increased to 40 mg/0.8 mL weekly.
Numerous publications have demonstrated the effectiveness of adalimumab in the treatment of uveitis associated with JIA, Behcet’s disease, Vogt-Koyanagi-Harada (VKH) disease, sarcoidosis, ankylosing spondylitis, birdshot chorioretinitis, pars planitis and idiopathic uveitis.
Indications for use are:
- Rheumatoid Arthritis
- JIA
- Ankylosing spondylitis
- Crohn’s disease
- Ulcerative colitis
- Uveitis
- Adalimumab is a fully human, recombinant immunoglobulin G, anti-TNF alfa
Contraindications - Severe infection, malignancies and pregnancy.
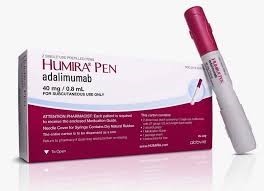
VISUAL 1 and 2 trials established the efficacy and safety of Adalimumab in active and inactive uveitis patients in a two-weekly dose.
3. Golimumab
It is a human monoclonal antibody acting against TNF-α which binds both the soluble and membrane forms of TNF. It was approved by the FDA in 2009 for the treatment of RA, psoriatic arthritis and ankylosing spondylitis and subsequently approved for ulcerative colitis. It is administered at a dose of 50 mg subcutaneously every month.
Golimumab was found to be effective in controlling recurrent and chronic noninfectious uveitis in GO- Easy study trial. It is less efficacious than adalimumab.
Etanercept – It is a humanised recombinant fusion protein (part TNF-α receptor and part Fc tail domain of human immunoglobulin G). Evidence suggests that etanercept has lower efficacy. etanercept for other indications It is not used commonly. Given subcutaneously and approved for use in JIA.
4. Rituximab
Rituximab is a chimeric monoclonal antibody specific to protein CD20, which is present only on mature B cells. When rituximab binds to B lymphocytes, it leads to apoptosis and a reduction in B cells lasting up to 9 months.
Rituximab has been used to treat Scleritis, JIA-associated uveitis, granulomatosis with polyangiitis with ocular and orbital involvement, anterior scleritis, and primary intraocular lymphoma. Infusion reactions and infectious complications, such as pneumonia and opportunistic infections are documented with the use of Rituximab.
5. Interferon
The interferons (IFNs) are a group of signaling proteins which activate immune cells. The use of IFNs for uveitis is documented in a case series of patients with refractory Behçet disease.
IFN treatment carries risks of flu-like illness, leukocytopenia, thrombocytopenia, anaemia, increased liver enzymes, increase in triglycerides, and allergic reactions.
- Tocilizumab – anti-IL 6 receptors (Posterior uveitis)
- Secukinumab – Anti IL 7 ab
- Daclizumab - IL 2 receptor antibody
- Certolizumab
D. Alkylating Agents
Chlorambucil and cyclophosphamide can be used as immunosuppressive agents but are rarely used as they cause mucositis, and bone marrow suppression and have a low therapeutic index. It is available in oral and injectable form. We need to titrate therapy to minimise side effects.
As these are strong chemotherapeutic agents and inhibit RNA and DNA synthesis in most of the cells, hence they are reserved mainly for malignancies like Retinoblastoma, Malignant melanoma, Leukemia and Lymphoma.
Nowadays lots of research is going on in the field of immunomodulators to treat uveitis. Still, one drug cannot be suitable for all. Individualised treatment needs to be tailored as per disease condition, severity and patients’ immune status and other organ system functions since all these drugs can affect different organ systems of an individual.
Bottom Lines
- Although many studies have documented the utility of biologics in the management of noninfectious uveitis, there are few studies to guide the recommendation of one biologic over another till now.
- These should be used with caution in immunosuppressed states like cancer, infectious disease, and diabetic patients. Live vaccines cannot be administered if these biologics are taken for any disease. Multiple sclerosis should also be ruled out. Besides common side effects of nausea, vomiting, rashes and itching patients can develop anaphylaxis with the use of these drugs.
- These drugs are effective in controlling recurrent and chronic noninfectious uveitis and have an established role in patients for whom steroids are contraindicated or ineffective. Their role in controlling posterior and intermittent uveitis is extremely beneficial and sight-saving. With the invention of newer molecules, the adverse effects of these drugs can be nullified.
- The use of these drugs in collaboration with rheumatologists saves sight of uveitic patients and avoids side effects of long-term usage of steroids, hence these will be the main drugs for uveitis treatment in the near future.
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr. Vandana Jain is a Senior Consultant at ESIC Hospital, Indore.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries