New orbital exenteration scoring system for mucormycosis
M3 India Newsdesk Jun 09, 2021
Just another complication that COVID-19 has brought our way is mucormycosis. This article throws light on the development of a grading system that a team of skilled otorhinolaryngologists and ophthalmologists have formed for considering orbital exenteration in mucor patients.
For our comprehensive coverage and latest updates on COVID-19 click here.
Introduction to mucormycosis
Humans are often exposed to mucormycosis fungus but seldom get illness due to their low virulence. It mostly affects immunocompromised individuals, with diabetes mellitus being, the most frequent risk factor. Other risk factors for mucormycosis include prior steroid treatment. However, during the COVID period, this lethal fungus produced an epidemic because of COVID-19's immunocompromising capabilities and the indiscriminate use of steroids for COVID therapy.
Inhalation of fungal spores or conidia is the most prevalent mechanism of dissemination for these fungi. Once within the tissues, these spores make their way to the blood vessels and become trapped there. This subsequently triggers an inflammatory response that results in the creation of a thrombus that grows in size and eventually compromises the blood flow to the tissues, resulting in ischaemic necrosis. Necrosis is what causes the blackening of the tissues that are associated with mucormycosis.
The initial symptoms seen by patients include impaired vision and monomuscular palsy resulting in diplopia, depending on the position of infection in the orbit and the tissue affected. On ophthalmoscopy, late characteristics include full blindness, chemosis/proptosis, total ophthalmoplegia, and optic atrophy. Continued intracranial spread may result in headaches, altered consciousness, and death.
Mucormycosis and the grading system
Mucormycosis is a fungal illness that spreads swiftly, is angioinvasive, and frequently deadly. The most essential choice in rhino-orbital mucormycosis therapy is whether to exenterate the orbit. Exenteration is frequently determined by the treating otolaryngologist and ophthalmologist. A novel scoring system has been devised that effectively monitors the disease's orbital involvement and also establishes the criteria for orbital exenteration in rhino-orbito-cerebral mucormycosis.
How does the grading system work?
A scoring system was developed by a team of skilled otorhinolaryngologists and ophthalmologists based on their past expertise with mucormycosis management. The grading system was developed around three primary criteria:
- Clinical signs and symptoms
- Ophthalmoscopy, direct and indirect
- Imaging analysis
The patients were scored using the scoring methodology. Surgical debridement from the nasal/paranasal/oral area and orbital exenteration were performed within 24 to 36 hours of admission, based on the score. Intravenous AmphotericinB was begun following a sensitivity test dosage of 1 mg/kg/day and maintained until a total dosage of 2 to 3 g was finished.
A second nasal endoscopy was done, and tissue from the probable diseased region was submitted to the pathologist for microscopic inspection on the KOH mount. AmphotericinB was discontinued if the KOH mount was confirmed to be negative. Patients were subsequently released and observed in the outpatient department.
Different points were assigned to various results based on their vision, salvaging ability of the eye, the chance of future spread, and cosmesis.
How the grade was assigned:
- 1 point = Minor symptoms/signs
- 2 points = Moderate symptoms/signs
- 3 points = Severe symptomatology/significance
- Clinical
- Opthalmology
- Imaging
Clinical symptoms
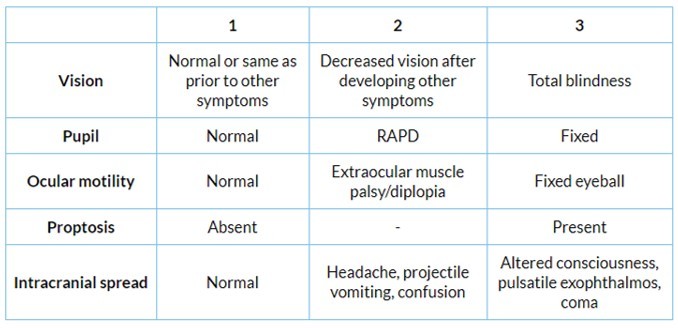
Ophthalmology
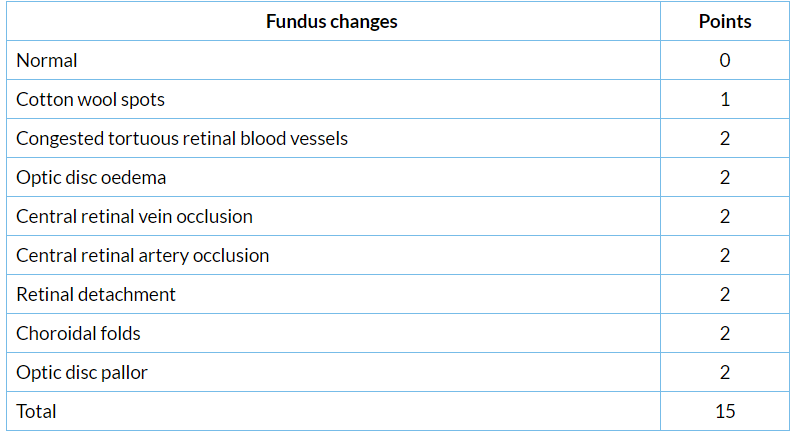
Imaging
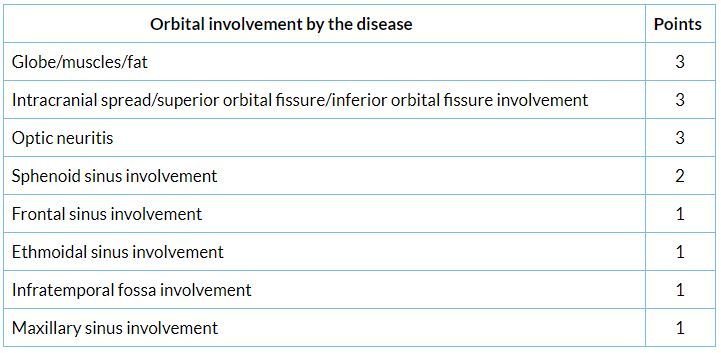 According to the scoring method, patients who scored greater than 23 were considered eligible for orbital exenteration, as approved upon by the otorhinolaryngologists and ophthalmologists. The majority of these individuals were discovered to have mucormycosis on histology and are presently stable following the conclusion of amphotericin therapy.
According to the scoring method, patients who scored greater than 23 were considered eligible for orbital exenteration, as approved upon by the otorhinolaryngologists and ophthalmologists. The majority of these individuals were discovered to have mucormycosis on histology and are presently stable following the conclusion of amphotericin therapy.
Treatment
The therapy of choice is surgical debridement of all necrosed tissue followed by injection amphotericin B (1 mg/kg/day for a total dosage of 2 to 3 g). However, when the orbit is involved, decision-making becomes more complicated. Vision is undoubtedly the most vital sense that a human being possesses. The choice to preserve or exenterate the eye during surgical debridement must be made collaboratively by the otolaryngologists and ophthalmologists.
- Exenteration of the orbit with enucleation
- Exenteration of the orbit endoscopically
- Amphotericin B
- Orbital reconstruction
The preceding section discusses the best treatment strategies for mucormycosis. The choice must strike a delicate balance between eye preservation and preventing the additional intracranial spread and, ultimately, death. New management choices include the following:
- Posaconazole was administered after six weeks of ineffective amphotericinB treatment and showed considerable clinical improvement as early as seven days into the treatment with continuous improvement for 23 weeks of therapy with no adverse effects related to posaconazole.
- HBO2 and GCSF are two more promising medicinal treatment alternatives. They work by increasing the capability of leukocytes to kill and increasing oxygen supply to the tissues. Their purpose, however, is only to supplement systemic antifungals.
The novel scoring system is an appropriate and encouraging tool for resolving the conundrum of orbital exenteration in rhino-orbito-cerebral mucormycosis. This scoring method, developed by a team of expert otorhinolaryngologists and ophthalmologists based on earlier experience with mucormycosis, is now widely used to determine the appropriate care strategy for the disease's new epidemic in the COVID pandemic.
Disclaimer- The views and opinions expressed in this article are those of the author's and do not necessarily reflect the official policy or position of M3 India.
The author is a practising super specialist from New Delhi.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries