New JAPI guideline for angina
M3 India Newsdesk Nov 08, 2021
A consensus statement about the comprehensive treatment of angina was published in the Journal of the Association of Physicians of India with the assistance of numerous meetings conducted throughout India. A thorough study of the literature, intensive debate and input from a number of cardiologists resulted in the creation of the statements on the definition, diagnosis, and treatment of angina, which have been summarised in this article.
Coronary heart disease
Coronary heart disease (CHD) has reached pandemic proportions worldwide. Increased interventional treatment and improved adherence to medicinal therapy have resulted in a 33% decrease in cardiac mortality five years following hospital discharge.
Angina pectoris is a frequent sign of coronary artery disease. Anti-ischaemia treatment aims to alleviate angina symptoms, improve exercise capacity and quality of life, improve prognosis, and avoid cardiovascular (CV) events in patients with stable coronary artery disease (CAD).
The consensus statement was drafted after many discussions conducted throughout India. Ten virtual meetings of the regional advisory board were conducted in Mumbai, Delhi, Chennai, Kolkata, Ahmedabad, Cochin, Trivandrum, Lucknow, Bhopal, and Varanasi.
Ten renowned cardiac specialists from each area attended these sessions. A consensus statement on the comprehensive treatment of angina was developed with the assistance of numerous meetings conducted throughout India and published in the JAPI: Journal of the Association of Physicians of India.
Anti-ischaemia treatment aims to alleviate angina symptoms, improve exercise capacity and quality of life, improve prognosis, and avoid cardiovascular (CV) events in patients with stable coronary artery disease (CAD).
Trends in coronary artery disease in India
- In 2012, cardiovascular disease (CVD) claimed 17.5 million lives worldwide. In the 1980s and 1990s, the Registrar General of India (RGI) estimated that CVD was responsible for 15% to 20% of fatalities in the nation. Annually, about 10.5 million people die in India, with CVD accounting for 20.3 per cent of male fatalities and 16.9 per cent of female deaths.
- According to the Global Burden of Diseases, Injuries, and Risk Factors research, CHD-related deaths and disability have more than quadrupled in India over the past three decades.
- Premature CHD is a growing issue in emerging nations such as India. According to the Million Death Study, India has a significant rate of early death owing to CVD. According to the Women's Ischemia Syndrome Evaluation (WISE) research, women had a lower incidence of obstructive coronary artery disease but a greater prevalence of coronary microvascular dysfunction.
- In women, obesity is a stronger risk factor for angina than it is in males. Microvascular angina affects 30% of individuals with stable angina who have normal coronary arteries. It is believed that approximately 40% of angina patients suffer from vasospastic angina.
- Increasing the use of interventional treatment and improving adherence to medicinal therapy has resulted in a 33% decrease in cardiac mortality five years following hospital discharge.
- Diabetes mellitus (DM) is a risk factor for atherosclerosis in and of itself, and coronary artery disease (CAD) is a common cause of morbidity and death in the diabetic population. Patients with diabetes mellitus had more extensive coronary disease and a worse rate of survival after acute myocardial infarction (AMI) than those without diabetes mellitus. However, studies indicate that individuals with diabetes often have asymptomatic (or "silent") ischaemia.
- Numerous studies have shown a greater prevalence of angina in individuals with diabetes mellitus compared to those without diabetes after an AMI.
Expert group recommendation 1
Definitions
- The terms stable angina/stable coronary artery disease has been superseded by chronic coronary syndromes (CCS).
- Coronary syndromes are classified as chronic coronary syndromes (CCS) and acute coronary syndromes (ACS).
- ACS is further subdivided into ST-elevation myocardial infarction (STEMI), non-ST-elevation myocardial infarction (NSTEMI), and unstable angina.
CCS is further classified as:
- Stable angina
- New heart failure (HF) and suspected CAD
- Stabilised symptoms for less than a year post ACS or PCI
- Stabilised symptoms for more than a year post initial diagnosis
- Patients with angina and suspected microvascular disease
- Asymptomatic CAD detected at screening
Expert group recommendation 2
Diagnosis
- Exclusion diagnoses include microvascular angina and vasospastic angina.
- If ischaemia is detected on resting electrocardiogram (ECG) and echocardiogram (ECHO) as well as stress testing, angiography should be performed.
Expert group recommendation 3
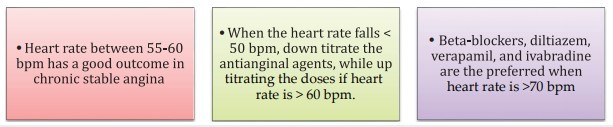
Heart rate management
Pharmacotherapy
Additional therapeutic options
- Counselling, ACE inhibitors, anxiolytics, and cholesterol and anaemia control are all critical components of CSA treatment.
- Statins have been proven to reduce secondary events and improve chest discomfort in patients with non-obstructive angina.
- Aspirin and statins are both recommended for microvascular dysfunction and have been shown to be the most beneficial.
- Anxiolytics have been shown to alleviate chest discomfort in some people.
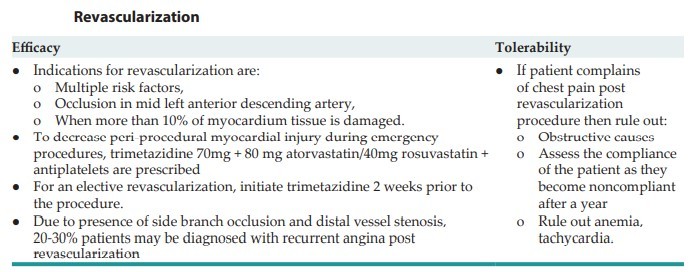
- Coronary revascularisation.
- Angina management in special populations.
Angina in hypotension and bradycardia patients
- Around 10% of individuals suffer hypotension and bradycardia, which results in a poor prognosis.
- Prescribing nitrates or beta-blockers to older patients may result in hypotension/bradycardia.
- To treat hypotension, modify the dosages of anti-anginal medications given and monitor for signs of left ventricular dysfunction.
Angina in diabetes patients
- Diabetes is detected in almost 50% of angina patients.
- Trimetazidine or ranolazine are recommended in individuals with diabetes mellitus who have systolic heart failure if angina continues after beta-blockers, nitrates, or calcium channel blockers.
- Ranolazine is favoured in diabetes patients because it significantly lowers glycated haemoglobin levels.
- In newly diagnosed diabetes patients, intensive diabetes management minimises both micro and macrovascular problems.
Newer therapies
- Newer developing antianginal treatments, particularly trimetazidine, should be preferred.
- Agents such as allopurinol, coronary sinus dilation, increased external counterpulsation, and neuromodulation is being explored for the treatment of CSA.
Click here to see references
Disclaimer- The views and opinions expressed in this article are those of the author's and do not necessarily reflect the official policy or position of M3 India.
The author is a practising super specialist from New Delhi.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries