New breath test may accurately diagnose esophagogastric cancer
M3 Global Newsdesk Jul 23, 2018
Researchers in the UK have developed a simple, noninvasive, and inexpensive exhaled breath test that shows promise in detecting esophagogastric cancer (EGC). Results of the study were published in JAMA Oncology.
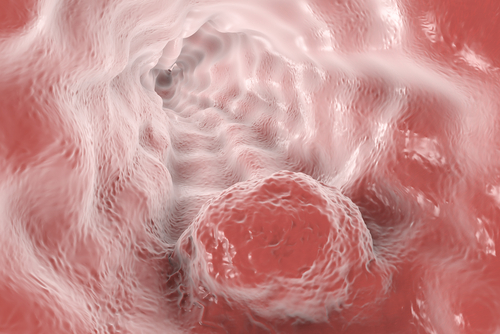
The symptoms of EGC are nonspecific, so many patients present with advanced-stage disease and have poor outcomes. Prior studies have shown that volatile organic compounds (VOCs) emitted in breath might be biomarkers for lung, bladder, and breast cancers. Sheraz R. Markar, PhD, MRCS, Imperial College, London, England, and colleagues evaluated VOCs in exhaled breath samples to determine the accuracy of a breath test for the diagnosis of EGC.
Five specific VOCs with good diagnostic accuracy, including butyric acid, pentanoic acid, hexanoic acid, butanal, and decanal, were assessed in exhaled breath samples using selected ion flow-tube mass spectrometry (SIFT-MS). Patients were consecutively recruited on a 1:1 cancer:control ratio from three London hospitals. Breath samples were returned to a central laboratory for analysis.
Patients with cancer were sampled when they were neoadjuvant-näive, had histologically confirmed nonmetastatic esophagogastric adenocarcinoma (stage I-III), and were on a curative treatment pathway. Controls were patients with benign gastrointestinal (GI) conditions or a normal upper tract.
Breath samples were collected using secure 500-mL steel breath bags and were analysed by SIFT-MS. Quality assurance measures included sampling room air, training all researchers in breath sampling, regular instrument calibration, and unambiguous VOC identification by gas chromatography mass spectrometry.
Data such as patient demographics, tumor characteristics, comorbidities, medications, and lifestyle measures, and endoscopy and/or surgery results were recorded for each patient. A total of 335 patients were included; 172 patients in the control group and 163 patients with esophageal or gastric cancer.
The majority of control patients (51.7%) had a normal upper GI tract on endoscopy or only the presence of a hiatal hernia. Other diagnoses were esophagitis, gastritis, duodenitis with or without erosions, benign gastric polyps, and achalasia or esophageal stricture.
Compared to controls, the cancer group had significant increases in patient age, proportion of male and white patients, ex-smokers, severe systemic disease (ASA classifications), and hypertension, and less liver impairment. Use of statins, β-blockers, and ACE inhibitors was also increased. Patients most often presented with dysphagia, vomiting, and GI bleeding, and less often with abdominal pain; 72 (44.2%) of the tumors were gastric in origin, 123 (69.3%) were T3 or T4, and 106 (65%) were nodal positive.
No adverse events were observed during breath sampling.
The concentrations of butyric acid, pentatonic acid, hexanoic acid, butanal, and decanal showed significant differences between the cancer and control groups, but there were no significant differences in the concentration of these VOCs between patients with esophageal or gastric cancer.
The VOCs were taken forward to form a risk-prediction model for the diagnosis of EGC which showed a good diagnostic accuracy with an area under the curve (AUC) of 0.85. This translated to a sensitivity of 80% and specificity of 81% for the diagnosis of EGC.
This compares favorably to existing technologies such as fecal occult blood test (sensitivity ranging from 30%-70%) for colorectal cancer, and the cytosponge (sensitivity 73%) for Barrett esophagus.
The authors admit that the study had limitations, such as the possibility of unmeasured confounding variables that can influence the changes in VOCs. In addition, up to 8% of diagnostic endoscopies can miss gastric and esophageal cancers, and most patients in the study had T3 EGC, so accuracy in identifying early stage cancer is not known.
“This multicenter study demonstrated a sensitivity of 80% and specificity of 81% of a single breath test in the diagnosis of esophagogastric cancer, thus validating the 5-VOC breath model,” concluded the authors, who noted that a large-scale diagnostic study is needed to determine accuracy in the primary care population.
To read more about this study, click here.
This story is contributed by Robyn Boyle and is a part of our Global Content Initiative, where we feature selected stories from our Global network which we believe would be most useful and informative to our doctor members.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries