NAFLD & NASH: What are the treatment strategies?: Dr. Manish Bhatnagar
M3 India Newsdesk Aug 25, 2021
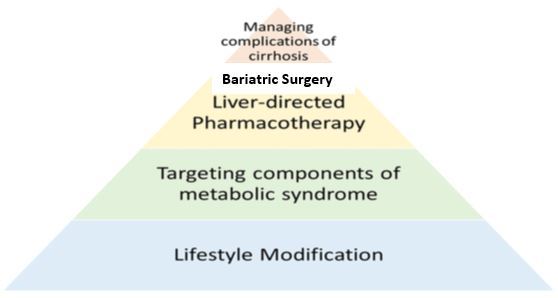
Dr. Manish Bhatnagar elaborates on the treatment pyramid for NAFLD- lifestyle modifications, pharmacotherapy and surgery options for managing progressive complications of the disease.
Key practice points
- NAFLD/fatty liver is the most common liver disease, frequently associated with insulin resistance.
- Meta-analytical data shows that NAFLD evolves towards liver cirrhosis and hepatic failure.
- Most so-called cryptogenic cirrhosis turns out to be underlying NAFLD. It is not an innocent bystander or a benign disease.
- NAFLD is to be searched for in overweight, diabetic patients and patients with altered liver enzymes.
- Treatment aims at normalising weight and lifestyle modifications are the key.
- Pharmacological treatment is evolving with new drugs on the horizon.
Treatment of NAFLD
The management of NAFLD should consist of treating liver disease as well as the associated metabolic comorbidities such as obesity, hyperlipidaemia and IR.
Treatment pyramid in NAFLD/NASH
Lifestyle modification
For treatment of NAFLD, lifestyle modification has been the mainstay of management which consists of diet, exercise and weight loss. Compliance with a calorie-restricted diet over the long term is associated with mobilisation of liver fat and improvement in cardiovascular risk. [1] A good recommendation is for patients to do 30 minutes of daily exercise. Another suggestion is to increase the daily step count to >10000 steps/day. Exercise increases skeletal muscle insulin sensitivity and so reverses insulin resistance which is one of the major mechanisms of NAFLD causation.
Targeting metabolic syndrome
1. Orlistat: It is an enteric lipase inhibitor that causes fat malabsorption thereby aiding weight loss and improvement in NAFLD/NASH. Sibutramine and Rimonabant are other options.
2. Statins: With antioxidant and anti-inflammatory properties, in addition to the frequent coexistence of NAFLD and dyslipidaemia, and the increased cardiovascular risk of these patients, statins appear as an attractive therapeutic option in NAFLD. Important evidence indicates the use of statins in order to reduce cardiovascular disease in patients with dyslipidemia. However, data on the effectiveness of statins for the treatment of NAFLD is scarce. So at the present time, when there is still a lack of evidence of any histological benefit, therapy with statins may not be recommended as primary therapy for NAFLD but as a treatment for associated hyperlipidemia.
3. Lipid-lowering drugs: Hypolipidemic medication such as statins and omega-3 fatty acids are seen as potential options for the treatment of NAFLD due to their effects on hypertriglyceridemia and low levels of HDL cholesterol, which are common changes in patients with metabolic syndrome.
Liver-directed pharmacotherapy
Omega 3 fatty acids
Omega 3 fatty acids, especially eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) are potent activators of nuclear receptor proteins such as PPARα and PPARγ, which regulate various genes involved in the stimulation of fatty acid oxidation, regulate pro-inflammatory genes, such as TNF-α and IL-6, and improve insulin sensitivity.[2,3]
In relation to the effects on NAFLD, a recent systematic review and meta-analysis found heterogeneity between the studies and concluded that, although omega-3 supplementation may decrease fat in the liver (without effects on transaminase levels), the optimal dose has not yet been established. [4]
Insulin sensitisers
Thiazolidinediones/ Metformin/ Incretin based therapies: Pioglitazone has been seen to improve liver histology in patients with and without Type 2 DM with biopsy-proven NASH. Therefore, it may be used to treat these patients. Before starting the therapy, patient counselling regarding the risks and benefits of the treatment should be discussed. The safety and efficacy of pioglitazone have not been established in the treatment of NAFLD.
Glitazones increase the synthesis and uptake of the fatty acids by the adipocytes, leading to fatty acids loading of the adipose tissue, instead of other organs, such as the liver and muscle.[5] They also upregulate adiponectin, an adipokine with anti-steatogenic and insulin-sensitizing properties.[6]
Pioglitazone has been shown to improve histological NASH in terms of steatosis, inflammation, ballooning, NAS score and resolution of NASH.[7] Due to side effects, especially cardiovascular and metabolic (weight gain), and because long term safety and efficacy of pioglitazone are not established, long term use of pioglitazone is under debate. However, for diabetic biopsy-proven NASH patients, pioglitazone may be considered.
Vitamin E
Vitamin E is a fat-soluble compound. It is part of the cell membrane and protects it from oxidative damage induced by free radicals.[8] It prevents liver injury by blocking intrinsic apoptotic pathways and by protecting against mitochondrial toxicity.[9] Vitamin E improves histological NASH in terms of steatosis, inflammation, ballooning, NAS score, and resolution of NASH at a dose of 800 IU/day.30 Its long term use is associated with increased all-cause mortality, increased incidence of hemorrhagic stroke and increased risk of prostate cancer.[10]
Cytoprotective agents
- Ursodeoxycholic acid-Ursodeoxycholic acid (UDCA) is an excellent example of a cytoprotective agent that has been investigated in the treatment of NASH. Randomised trials now suggest that UDCA is not effective.
- Obeticholic acid- Obeticholic acid is a potent activator of the farnesoid X nuclear receptor (FXR). Once activated in the liver, FXR reduces bile acid synthesis, improves insulin sensitivity and decreases gluconeogenesis, and reduces inflammation, lipogenesis and fibrosis.[11] Obethicolic acid, 25mg/day for 72 weeks, for non-cirrhotic NASH, has been shown to improve all histological lesions of NASH, including fibrosis.[12]
- Pentoxifylline- Another approach to the treatment of NAFLD involves using anti-TNF-α drugs, given that this cytokine induces both necroinflammation as well as insulin resistance.[13] A meta-analysis assessing five randomised, placebo-controlled studies, including only 157 patients, showed that pentoxifylline can reduce transaminase activity and improve histological parameters in NAFLD patients.[13]
- Saroglitazar- It is a novel category of drug being used in NAFLD/NASH with promising results. It has shown definite promise in treating diabetic dyslipidaemia.
Management of underlying metabolic risk factors
All patients with NAFLD require treatment of associated metabolic risk factors, such as diabetes, hypertension and dyslipidaemia.
- The treatment of patients with type 2 diabetes and NAFLD can include metformin, pioglitazone, GLP-1 agonist, insulin or sulfonylureas.[7]
- Antihypertensive medications can bring additional benefits, besides lowering hypertension, when there are used blockers of the renin-angiotensin-aldosterone system, and in particular, sartans.[10]
- Statins are safe to use in the NAFLD population.[11]
Bariatric surgery
All appropriate non-surgical measures must be tried before surgery is offered to the patient. The NICE guidelines suggest surgery as the first-line option only if BMI >50Kg/m2.
In patients with morbid obesity or obese patients of greater severity (BMI >40 or BMI between 35 and 40 with comorbidities), bariatric surgery induces long-term maintenance of weight loss and has been recommended by the researchers for motivated candidates. Whatever the surgical procedure, 14 to 25% weight loss is observed 10 years after surgery, associated with improvement in IR, remission of diabetes mellitus and few cardiovascular events. [12,13] It should be considered that although bariatric surgery may play a role in the treatment of patients with morbid obesity and NASH, the recommendation of this procedure must be individualised and conducted at specialised medical centres with a multidisciplinary approach due to the potential complications, which vary depending on the centre where the procedure is performed.[14]
Management of complications of cirrhosis
The suggested strategy is:
- HCC: Six-monthly Sonography + AFP.
- Varices: Banding + Annual surveillance Gastroscopy.
- Osteoporosis: Correction of vitamin D/calcium deficiency. BMD testing is advisable.
- Liver transplant in patients with advanced cirrhosis.
Conclusion
Lifestyle interventions aimed at weight loss and increased activity are essential for all patients with NAFLD and if sustained is effective in the treatment of NAFLD. For patients who fail lifestyle intervention, liver-directed pharmacotherapy with pioglitazone or vitamin E can be considered for those with advanced, but pre-cirrhotic NASH. Features of metabolic syndrome and cardiovascular risk factors are very common in NAFLD, so all patients should be screened for these and have them managed aggressively. For patients who develop advanced disease, they require surveillance for and management of the complications of cirrhosis (HCC, varices, osteoporosis).
Click here to see references
Disclaimer- The views and opinions expressed in this article are those of the author's and do not necessarily reflect the official policy or position of M3 India.
The author, Dr. Manish S Bhatnagar is a Consultant Gastroenterologist, Hepatologist and Therapeutic Endoscopist from Ahmedabad.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries