Rise of Monkeypox: Presenting to You Some Myth-Busters, Preventive Strategies and Treatment Options
M3 India Newsdesk Aug 25, 2022
Before the recent pandemic scare in India was wiped and washed completely, the healthcare professionals came across another challenging situation. In this article, the author discusses monkeypox, its communicability, treatment and prevention.
What is monkeypox?
Monkeypox (MPX) is a rare condition caused by the monkeypox virus, which is a part of the same family of variola virus, which causes Small Pox (SP). There is a similarity between the symptoms of MPX and SP, but MPX is more fatal and is not related or has any clinical significance or similarity with chicken pox.
Monkeypox has raised many questions among the common people and the healthcare fraternity. As of June 2022, with 3413 confirmed laboratory cases, monkeypox has emerged to be the new healthcare scare all across the globe.
With myths like monkeypox emerges from monkeys and they spread it, to it being a variant of coronavirus, and the fact that this condition occurs only in a specific population due to some superstitious beliefs, lets us try and understand the depth of the condition by debuting these myths and explore the scientific facts associated with it.
Historical notions of monkeypox
This condition was discovered in 1958 when two outbreaks of pox-like diseases were recorded among the colonies of monkeys that were utilised for research. The first human case of MPX was reported in the 1970 Democratic Republic of the Congo.
Geographical distribution
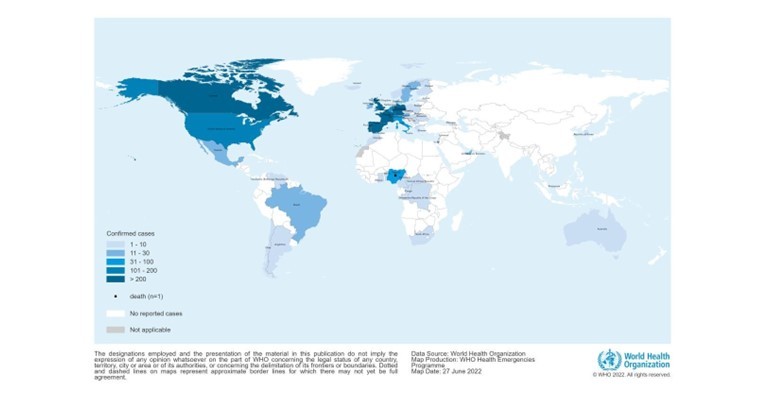
Before the recent outbreak, MPX was reported in several central and western African countries. The incidence was on a higher side in these countries and any cases outside Africa were always related to either foreign travel or imported animals from these regions. The image below represents the geographic distribution of cases between 1st January to 22nd June 2020.
Among the recent cases reported (3413), 86% of cases were reported from the European region and 11% cases were seen in the American region. Just about 2% of cases were seen in the African region and less than 1% of cases in the Eastern Mediterranean and Western Pacific Region. Only one death was reported to date and that was in Nigeria. India has also recently been under the radar with few reported cases in Kerala, Rajasthan and Delhi.
Host and agent
Some rodents like rope squirrels, dormice, and Gambian pouched rats are known to be naturally susceptible to the virus but their natural habitat is still unknown. Monkeypox virus (MPXV) belongs to the orthopoxvirus genus of the poxviridae family and has structurally double-stranded DNA The two distinct genetic clades of the MPXV - the Central African (Congo Basin) clade and the West African clade have been identified, The congo basin clade has historically caused more severe disease and was thought to be more transmissible and it is only the country of cameroon where both these were found. Endemic monkeypox is generally self-limited, with clade-dependent case fatality rates of 1 to 10%
Mode of transmission
The spread of this virus is directly related to close contact with an infected animal, human or any other material contaminated with the virus. The common routes of transmission are:
- Broken skin (Even if is not visible)
- Respiratory tract
- Mucous membrane (eyes, nose and mouth)
In terms of physical contact the modes of transmission could be:
- Sexual activities (as this can lead to direct contact with the monkeypox lesion or scab if one of the individuals is infected).
- Coughing or sneezing by an infected individual can pose a high risk for people around as it can be easily transmitted.
- Contact with the clothing or linens of an infected individual.
Animal-to-human transmission can also occur in the case of a bite or scratch done by an infected animal on a healthy human.
Period of incubation and communicability
The period of incubation is usually between 5-21 days and communicability is from 1-2 days before the rash appears to until all the scabs fall off or subside in proportion. As its a self-limiting disease, most individuals recover within a few weeks,
Clinical features
The beginning of the condition marks the presence of the following clinical features:
- Fever and chills
- Headache
- Bodyache and generalised malaise
- Joint pain
- Swollen lymph nodes
- Sore throat, nasal congestions or other respiratory symptoms like a cough
- Nausea/Vomiting
- Itching and pain concerning the skin rashes
The most distinct clinical feature is the development of the rash and it is typically seen at the:
- Areas like hands, feet,(palms and sole), face or mouth (95-98%)
- Genitals (penis,testicles,labia and vagina) (28%)
- Conjunctiva (20%)
The initial appearance of the rash is similar to a blister or a pimple and in a few cases can be itchy and painful. These skin rashes typically develop within 1-3 days of fever onset and last for around 2-4 weeks. They are deep-seated,well-circumscribed in nature and often develop umbilication. Initially, it starts as a simple rash and progresses toward umbilication through stages where the rash becomes papular around the 3rd day, vascular by the 4th to 5th day and pustular and sharply raised by the 6th to the 7th day. By the end of the 2nd week the rash dries up, and crusts and scabs remain for a week before starting to fall off the lesion.
The skin conditions are greatly based on various confounding factors like age, vaccination status, nutritional balance of the individual and any associated risk of HIV status. It occurs in communities most commonly with a higher prevalence of malnutrition, parasitic infections or general immunocompromised individuals due to some existing co-morbidities. An individual may develop a few or all of the symptoms depending on the degree of infection.

Treatment
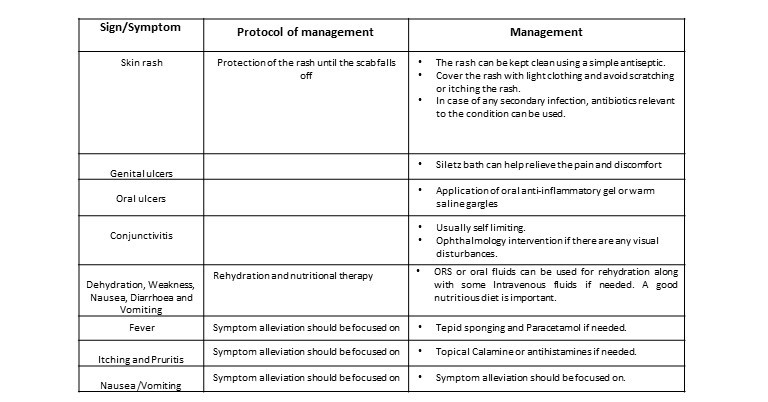
There is no specific treatment for MPX as of now but a proper approach to treat the patient symptomatically can act as a great method to alleviate the pain and discomfort and does propagate a good healing and faster recovery. Patient isolation and rehydration therapy are the two most important steps in the management of such patients. Isolation and wearing a triple-layer mask should be continued till the respiratory symptoms subside and all lesions have subsides and scabs have fallen off completely. Covering the skin lesions is of utmost importance to prevent the risk of contact with others. Vaccination against smallpox was demonstrated through several observational studies to be about 85% effective in preventing monkeypox.
The treatment protocol has been summarised in the following table :
Complications
Vigilant monitoring of these symptoms is extremely important to avoid any serious complications watch out for:
-
Shortness of breath, chest pain and difficulty in breathing
-
Altered consciousness
-
Seizure
-
The blurring of vision or any associated pain
-
Decrease in urine output
-
Extreme lethargy
- Secondary infections like pneumonia, sepsis, encephalitis etc.
Prevention and infection control
A proper regimen for isolation of both patient and healthcare provider should be taken care of to avoid the transmission at a faster rate
- Isolation of infected individual.
- Wearing a mask at all times and also proper coverage of the infected skin lesions.
- Use of Personal Protective Equipment (PPE) by the healthcare professionals during all processes like sample collection and delivery of the treatment to the infected individual.
- All the laboratories handling the samples must be informed to ensure the appropriate control and measures are taken to minimise the risk of transmission among the laboratory workers.
- Appropriate tracking should be done by the local authorities in collaboration with healthcare providers to assure the isolation of patients in the early stages.
Click here to see references
Disclaimer- The views and opinions expressed in this article are those of the author's and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr Ridima Surve is a practising dentist from Mumbai.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries