Exploiting the Use of Medicines can Worsen Headaches: Understanding Medication Overuse
M3 India Newsdesk Oct 05, 2022
Medication Overuse Headache (MOH) is a neurological disorder which is characterised by repetitive episodes of headache which eventually turns into a chronic condition because of overuse of medications. In this article, the clinical management of MOH will help physicians in their regular practice.
Key takeaways
- The diagnosis and treatment of MOH can be difficult tasks and requires a lot of exclusion-based diagnoses and in-depth history taking of the patient.
- The rate of relapse of MOH is quite high after the first 12 months of treatment and lies between 20-40%. But the prognosis based on this point can vary depending on the baseline primary headache and also other confounding factors. Hence regular follow-ups and treatment modulation is necessary for a better prognosis.
- A consensus protocol for the management of MOH, established through a study in 2014 stated that:
- There should be continuous advice on medication withdrawal given to the patient through a continuous and effective communication
- Plan early discontinuation with supportive treatment with withdrawal headache.
- Implementing a symptomatic treatment without using the drug that was previously overused.
- A follow-up every six months is highly recommended.
- Advising the patients to reduce consumption of caffeine and any other form of tobacco.
- Advising patients to work on increasing physical activity.
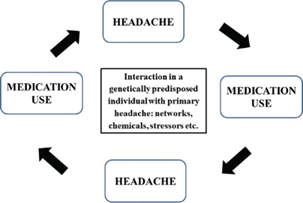
MOH becomes a vicious cycle as the patients consume medications to eliminate the headache but instead, there is an increase in the headache frequency. In short, the treatment for headaches becomes the cause for the same.
How is MOH diagnosed?
According to International Classification for Headache Disorders (ICHD-3) (2018), MOH is classified as a secondary headache or a chronic headache syndrome to a preexisting headache disorder. As the primary headache in patients with MOH, most of them have either of the below:
- Migraine
- Tension-type headache
- Or both of the above
A few patients have a primary headache as:
- Chronic Cluster headache
- New daily persistent headache
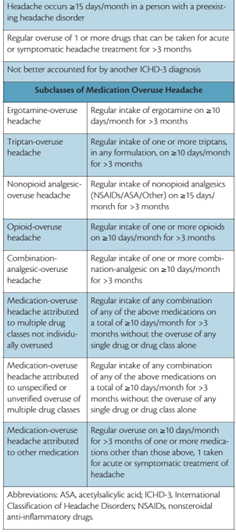
MOH will mostly occur after the primary headache and has some criteria which can help us understand the occurrence of this condition:
- Headache occurring on ≥15 days/month in a patient with a preexisting headache disorder.
- Regular overuse for >3 months of one or more drugs that can be taken for acute and/or symptomatic treatment of headache.
- Not better accounted for by another ICHD-3 diagnosis.
History and epidemiology
- The first case of MOH was seen in the 1930s when ergotamine was being used by people to treat headaches and this population showed signs of MOH when they overused it beyond a certain period.
- In 1951 a case series described the initiation of MOH when the use of ergotamine and remission of headache after its withdrawal.
- In 1988, ICHD described the term drug-induced headache after the excessive consumption of mostly ergotamine and analgesics.
- After a period of time when more drug classes came into the picture under this entity, the umbrella of MOH also included the overuse of simple analgesics and their combinations, opioids and triptans.
Incidence and prevalence of MOH
The prevalence of MOH in the general population is 1-2% and the male-to-female ratio is 1:3-4. It is more prevalent in individuals in their forties.
The prevalence of MOH in adolescents is only 0.3-0.5% and it is observed that the incidence of MOH decreases after the age of 60 years. The incidence of MOH in India is much less compared to the West which may be due to the common use of complementary and alternative medicine which is not classified and defined scientifically.
Classification of MOH
These headaches are classified according to their causative agent, the number of times these drugs are consumed and the total duration they are taken beyond the safety window.
Pathogenesis
The mechanism of how MOH occurs still remains unclear as the fact that the overuse is a consequence for individuals living with a chronic headache or the other way round. However not all individuals who have headaches develop MOH because of overuse. The pathogenesis of MOH will vary as per the class of drug that is being overused. Some proposed mechanisms have been stated in the past literature which can be the probable ones.
- Central sensitisation due to overuse of medications leads to neurological imbalance.
- Secondary to overuse of medication can lead to cortical neuronal hyperexcitability.
- Low serotonin levels can also be a cause of the development of MOH.
- Alteration in endocannabinoid systems.
- Some neuroimaging studies have also shown changes in the orbitofrontal cortex and mesocorticolimbic dopaminergic pathways.
- In the case of chronic exposure to opiates, increased expression of calcitonin gene-related peptide has been demonstrated in dorsal root ganglion neurons.
- Chronic use of morphine can alter the Diffuse Noxious Inhibitory Controls (DNICs) and impaired DNIC’s are found in MOH.
- A recent study showed the presence of candidate proteomic markers in the serum of patients with MOH which is also a similar finding in patients with chronic painful conditions.
Which medications can lead to MOH?
There are certain classes of drugs which are more prone to cause MOH when taken for a particular period and eventually exceeding the safe period dosage.
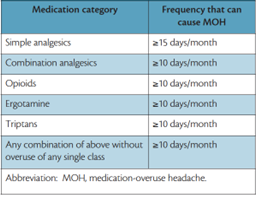
In the Indian scenario, the most commonly overused drug is a combination of caffeine 100 mg, of ergotamine 1 mg, paracetamol 250 mg, and prochlorperazine 2.5 mg, which contains ergotamine.
Risk factors
A study conducted in 2012 identified several risk factors of MOH in patients with a history of chronic headaches (an analysis was done with an 11-year follow-up. Also, a longitudinal study conducted in 2003 concluded that patients consuming analgesics daily or weekly at baseline have a higher risk of developing chronic headaches 11 years later.
A few risk factors are listed below:
- Regular use of analgesics/tranquillizers
- History of previous primary chronic headaches like migraine and tension-type headaches
- Chronic musculoskeletal disorders
- Gastrointestinal complaints
- Lack of physical activity
- Smoking
- Depression and Anxiety
Clinical features of MOH
- Nature: Refractory, severe in nature at times
- Location: This may vary on different days
- Frequency: Almost daily leading to extreme discomfort at times
It is associated with other clinical features like:
- Nausea
- Asthenia
- Irritability
Loss of focus and difficulty in concentration.
- Anxiety and depressive mood
- Patients using ergotamine may have
- Cold extremities
- Tachycardia
- Hypertension
- Muscle pain
Diagnosis and investigations
- Taking a detailed history of any preexisting headache or history of the same should be done with a special emphasis on the duration, frequency, and dosage of the medications used by the patients for the treatment of primary headaches.
- The ICHD-3 criteria can be treated as a gold standard in diagnosing MOH during history taking.
- A physical examination is a must to rule out the secondary causes of the headache by looking at features like focal deficits and papilledema.
- To rule out any lesions in the central nervous system by conducting imaging like Computerised Tomography (CT) and Magnetic Resonance Imaging (MRI) which might also mimic e a chronic headache.
Differential diagnosis
- Chronic Migraine
- Chronic Tension-type Headache
- Hemicrania continua
- Idiopathic Intracranial Hypertension
Treatment
The diagnosis of MOH and the following treatment can be extremely challenging and requires good patient compliance too. The treatment management strategy will revolve around these three goals:
- Meticulously plan the withdrawal of the causative overused drug.
- Provide the required symptomatic pharmacological and non-pharmacological treatment.
- Prevent relapse.
Withdrawal can be abrupt or gradual. For drugs, like triptans, ergotamines and simple analgesics the withdrawal can be abrupt but for opioids, barbiturates and benzodiazepines, a tapered withdrawal is suggested. A few patients can also develop withdrawal symptoms such as headaches, nausea and vomiting, irritability, sleep issues, hypotension, restlessness and anxiety. The duration of these symptoms can last for a few days or can continue for a few weeks.
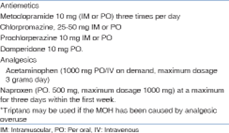
The question is how can one deal with the headaches in the withdrawal phase?
It is recommended that these headaches can be treated with some acute medications ensuring that the medications which were being overused earlier are being avoided now.
The drugs used in the treatment of withdrawal headaches are mentioned below:
Patient education is again a very important factor in the treatment of MOH. Patients should be rightly educated about the side effects due to overuse and should be cautiously warned to take medications as per the prescribed dosages and in the right combinations. In this process, it is also important to educate the pharmacists to avoid disposing of medications over the counter (OTC).
Disclaimer- The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr Ridima Surve is a practising dentist from Mumbai.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries