Local anesthesia reactions: How to treat?
M3 India Newsdesk Oct 08, 2021
Local anaesthetics are extremely safe drugs when used as recommended. However, every drug has the potential for producing unwanted and undesirable effects. This article will highlight the causes, signs and symptoms of the common complications of local anaesthesia and their management.
Practice pearls
- The complications from local anaesthesia can easily be prevented, provided the operator is aware of the management guidelines and is able to recognise the signs and symptoms of allergy and toxicity to the drug
- Evaluation of the patient before administration of LA is a pre-requisite. Anxiety, fear and apprehension need to be managed beforehand
- The lowest effective concentration of LA should be administered and at a slow speed, preferable for a duration of 1 minute
- Observe the patient both durRing and after LA administration for signs and symptoms of undesirable reactions
Local anaesthetics (LA) are drugs used for minor surgical procedures which do not cause loss of consciousness. They are helpful in procedures such as:
- Minor surgical procedures on the skin such as removal of warts, moles, etc.
- Some eye surgeries such as cataract removal
- Biopsy of lesions
- Dental procedures such as extractions, fillings and root canal treatment
Local anaesthesia has very few complications as compared to general anaesthesia, although, sometimes there can be reactions such as:
- Allergy to local anaesthesia
- Toxicity or local anaesthesia poisoning
Hypersensitivity to LA
Signs and symptoms of an allergic reaction to LA can range from mild to severe, immediate to delayed. Immediate reactions develop within seconds to hours of exposure to LA. The most frequently involved areas are the skin, respiratory system, cardiovascular system and mucous membranes. Reactions can be:
- Cytotoxic: Transfusion reactions, haemolytic anaemia, autoimmune haemolysis
- Immune complex reactions: Manifested within 6 to 8 hours as serum sickness, acute viral hepatitis, nephritis
- Anaphylactic reactions: Affects skin and mucous membranes, gastrointestinal, cardiovascular and respiratory systems
The most commonly occurring immediate reactions include urticaria and angioedema.
- Urticaria presents as smooth or elevated patches of skin along with intense itching.
- Angioedema presents as localised swelling in the region of lips, tongue, face, larynx and pharynx.
The second most common reaction involves asthmatic reactions which present as prolonged expiration along with wheezing sound.
Generalised anaphylaxis may also occur in some patients which presents as cardiovascular and respiratory collapse. It is generally accompanied by severe pruritis, erythema and urticarial, nausea, vomiting, diarrhoea and gastrointestinal discomfort. Airway oedema along with wheezing and dyspnoea may occur. This can further be accompanied by a decrease in heart rate, hypotension and ultimately cardiac arrest. In some cases, death may also occur in minutes.
Delayed reactions usually occur 48 hours following the administration of LA. It can be presented as localized oedema, malaise and tenderness in the area of injection.
Management of allergic reactions
- Diphenhydramine orally 50 mg every 3 to 4 hrs; in case of mild localised reactions
- Diphenhydramine IV/IM 25 to 50 mg or Epinephrine SC/IM 0.3 to 0.5mg (0.3-0.5 ml of 1:1000 Adrenaline); in case of severe yet localised reactions
- Dexamethasone IV 4 to 8 mg; in case of severe reactions
- 100% oxygen and Aminophylline IV 0.5 g for patients experiencing respiratory distress
Local anaesthesia toxicity
Toxicity/toxic overdose occurs when the concentration of drug administered can sufficiently affect the circulatory, respiratory and central nervous systems. Inadvertent IV injections of LA has been recorded as the main cause of toxic reactions wherein LA gets absorbed into the intravascular system at a greater rate than the rate of its biotransformation.
The cardinal rule of regional anaesthesia is to “aspirate before injecting”. However, a negative aspirate is not a guarantee of the needle not being lodged in a blood vessel. High blood viscosity and occlusion of the needle by a collapsed vessel wall may also lead to a negative aspirate. Hence, the safest way out is the slow deposition of LA.
Usually, CNS stimulation occurs, followed by depression. However, CNS depression may also occur as the first sign of toxicity. CNS stimulation presents as restlessness, apprehension, talkativeness, excitement and even convulsions. CNS depression is presented as sleepiness, lethargy and unconsciousness. These reactions are accompanied by increased pulse rate, blood pressure, respiratory rate. Vomiting and nausea may also occur.
Prevention of LA toxicity
- An appropriate anaesthetic agent must be selected
- Use of a vasoconstrictor along with LA is advisable as it prolongs the action of LA, slows its absorption and permits smaller volumes of LA to have efficient action
- The least possible volume of LA should be used
- Aspirate before injecting
- There should be slow and controlled deposition of LA
Management of LA toxicity
- Patients who are mildly stimulated do not require any treatment. Discontinuation of further administration of LA is a necessity. Moderately stimulated patients need to be administered pentobarbital sodium IV very slowly along with oxygen supply until they calm down.
- Convulsive patients should be given succinylcholine chloride IV 20 to 50 mg or Midazolam IV 1 mg/min or IM 5 mg/ml.
- In case hypotension extends 30 minutes, administer ephedrine.
- Basic emergency management protocol to be followed: P→A→B→C→D i.e., the position of the patient; maintenance of airway; assess breathing, provide ventilation if needed; provide cardiac compressions, if needed and provide definitive emergency drug administration.
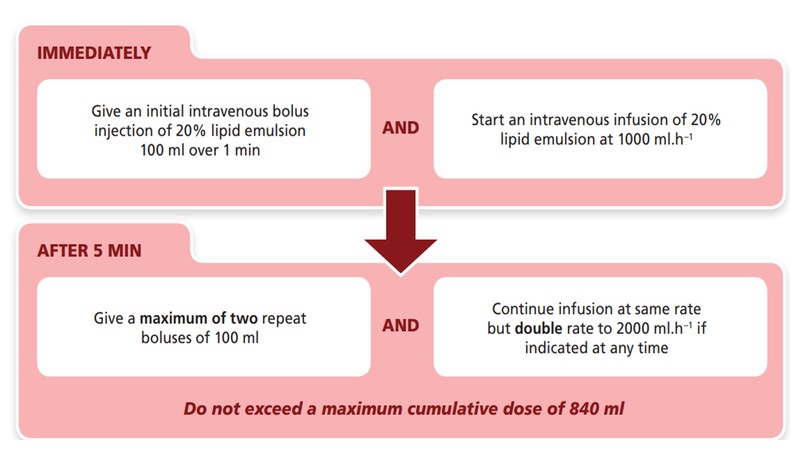
Summary of management of LA toxicity
As per the Association of Anaesthetists of Great Britain, an approximate dose regimen for a 70-kg patient would be as follows:
Summary of management of anaphylactic reaction
As per the Australian Academy of Clinical Immunology and Allergy, treatment protocol involves:
- Primary treatment: IV fluids (25–50 mL/kg of crystalloid solution)
- Epinephrine intramuscular
- Autoinjection of 1:1000 solution
- Weight 10–25 kg: 0.15 mg epinephrine IM (deltoid or vastus lateralis) autoinjector or needle
- Weight >25 kg: 0.3 mg epinephrine IM (deltoid or vastus lateralis) autoinjector or needle
- Repeated doses of epinephrine may be needed every 5–15 minutes
- Epinephrine intravenous (for profound bronchospasm or hypotension)
- Use epinephrine 1:10,000 in a prefilled syringe for IV use
- Begin at dose of 50–200 mg IV (0.5–2 mL), increase as needed
- Epinephrine intramuscular
- Secondary Treatment
- Bronchodilator (b2-agonist)
- Albuterol (90 mg per inhalation puff)
- H1-blocker (antihistamine)
- Diphenhydramine (Benadryl) (IV 0.5 mg/kg), requires dilution to avoid vein damage
- Optional H2-blocker
- Famotidine (Pepcid) (20 mg IV)
- Hydrocortisone (1–2.5 mg/kg)
- Methylprednisolone (1 mg/kg)
Click here to see references
Disclaimer- The views and opinions expressed in this article are those of the author's and do not necessarily reflect the official policy or position of M3 India.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries