Irritable Bowel Syndrome Management- How Indian Patients Differ
M3 India Newsdesk Apr 13, 2023
The Indian Neurogastroenterology & Motility Association has developed evidence-based guidelines for the management of Irritable Bowel Syndrome (IBS) due to its prevalence, negative impacts, & recent advancements in understanding the condition in India. Read those recommendations in this article.
Irritable bowel syndrome (IBS) is a prevalent ailment that has a negative influence on patients' quality of life and causes considerable morbidity, job absence, lost productivity, and economic cost to society.
In India, there have been a number of recent advancements in the knowledge of the pathogenesis, diagnosis, and treatment of IBS.
Also, India has a very distinct medication market from the rest of the globe. Also variable is how doctors in India practice. In order to address irritable bowel syndrome, the Indian Neurogastroenterology and Motility Association (INMA), formerly known as the Indian Motility and Functional Disease Association, created these evidence-based practice recommendations (IBS).
Expert panel assertions
Consensus opinion 1: In both clinical settings and the Indian population, IBS is a frequent ailment.
Consensus opinion 2: In India, IBS affects both males and females equally.
Consensus opinion 3: IBS patients in India often have other overlapping FGIDs (Functional Gastrointestinal Disorders).
Consensus opinion 4: Etiopathogenesis of IBS is multi-dimensional including gut-specific mechanisms, altered gut-brain interaction, food intolerance, and psychosocial and genetic factors.
Consensus opinion 5: Patients with IBS, particularly those with diarrhoea-predominant IBS (IBS-D), are more likely to have SIBO and gut dysbiosis.
Consensus opinion 6: Excessive methane production slows gut transit and is associated with constipation-predominant IBS (IBS-C).
Consensus opinion 7: Gastrointestinal infection with varied pathogens may result in post-infection IBS (PI-IBS).
Consensus opinion 8: A diagnosis of PI-IBS by Rome criteria does not exclude underlying post-infectious malabsorption syndrome (tropical sprue).
Consensus opinion 9: COVID-19 may lead to post-COVID-19 IBS.
Consensus opinion 10: Psychological and somatoform comorbidities are common in IBS.
Consensus opinion 11: Dietary FODMAPs (fermentable oligo-, di-, monosaccharides and polyols) may contribute to symptoms of IBS.
Consensus opinion 12: Diagnosis of IBS is primarily clinical and based on well-defined symptom-based criteria.
Consensus opinion 13: Rome III criteria may be preferred over Rome IV to diagnose IBS in India due to its higher sensitivity.
Consensus opinion 14: Rome’s subtyping of IBS into constipation and diarrhoea-predominant conditions frequently leads to a large proportion of patients remaining unclassified in India.
Consensus opinion 15: Bristol stool form scale (BSFS) along with other symptoms such as straining, incomplete evacuation, urgency and patient-reported bowel pattern should be assessed to evaluate bowel movement.
Consensus opinion 16. A: In the absence of alarm features, a few baseline investigations are suggested for patients with suspected IBS.
Consensus opinion 16. B: The presence of alarm features necessitates diagnostic tests to rule out organic disease.
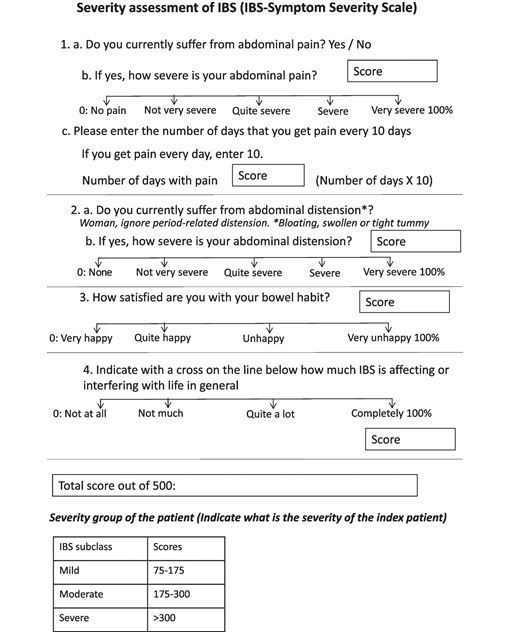
Consensus opinion 17: The multi-dimensional clinical profile of IBS needs to be incorporated into clinical practice, as proposed in the Rome IV algorithm.
Consensus opinion 18: Patients with refractory IBS symptoms need further pathophysiological evaluation.
Consensus opinion 19: Counselling, reassurance and lifestyle modification are important in the management of IBS.
Consensus opinion 20: The initial treatment of IBS is primarily symptom-based.

Consensus opinion 21: Antispasmodics are the first-line treatment of abdominal pain in patients with IBS and non-responsive patients may benefit from visceral neuromodulators.
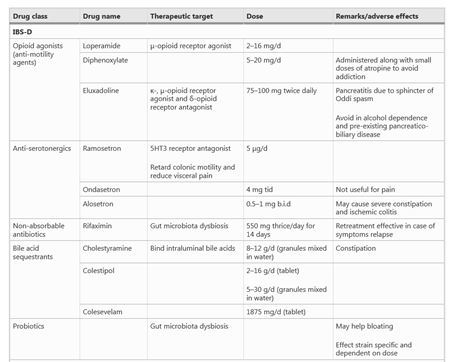
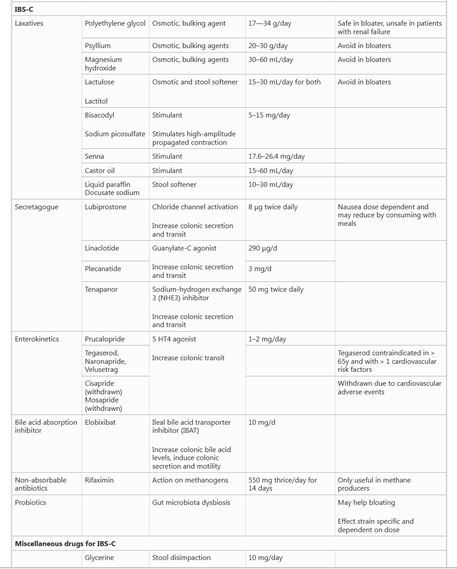
Consensus opinion 22: Laxatives and antidiarrheals are the first-line treatment for IBS-C and IBS-D, respectively.
Consensus opinion 23: Dietary FODMAP restriction is useful in a proportion of IBS patients.
Consensus opinion 24: Probiotics may be helpful but more studies are needed.
Consensus opinion 25: Non-constipated and methane-producing IBS-C patients benefit from rifaximin.
Consensus opinion 26: Pathophysiology-directed therapy is important in the management of refractory IBS.
Consensus opinion 27: Psychological interventions are useful in those with psychiatric comorbidities or refractory IBS.
Consensus opinion 28: Overlapping functional GI disorders may require combination treatment.
For further details, readers are requested to go through the following reference.
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr Monish Raut is a practising super specialist from New Delhi.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries