How will You Approach a Patient with Breathing Difficulties?
M3 India Newsdesk Jun 28, 2023
Acute dyspnea is among the most frequent causes of hospital emergency department admissions. The assessment, evaluation and diagnosis of dyspnea along with a case study are discussed in this article.
Medical professionals usually need to make a rapid and accurate ton to develop a treatment plan for acute dyspnea. It may be challenging to distinguish between a pulmonary and cardiac cause of dyspnea when a patient presents to the emergency room because their medical history and information are limited. Additionally, the pathophysiology may not be well defined by history and examination. Due to a delay in getting a definitive diagnosis, life might be lost since emergency room patients are often sicker patients.
A case of dyspnea
A 64-year-old lady who complained of respiratory problems was taken to the ER. Her vital signs were BP 192/106, HR 121, RR 32, and SpO2 86% on room air while she was being transported. She is breathing rapidly, and her shoulders and belly are moving in time with each breath. How should you approach a patient who is having breathing difficulties?
Introduction
Visiting the emergency room because of difficulty in breathing is a typical occurrence. After chest discomfort, the top five causes for hospital admission in individuals 45 years of age and older are:
- Pneumonia
- COPD exacerbation
- Heart failure exacerbation
- Dysrhythmias
Finding the underlying reason for shortness of breath is challenging since many different illnesses, including all of the aforementioned, may cause it. It is a vague symptom with a wide range of potential causes and degrees of severity, making it difficult to assess these people. Treatment and stabilisation often take place before a definitive diagnosis is made. When evaluating a patient, it's crucial to take into account the crucial diagnosis and keep an eye out for trends in the history and physical exam. Additional testing may be useful in confirming a diagnosis or ruling out other possibilities.
Actions at the outset and the first assessment
Overall perception
Patients who first come with shortness of breath as their primary symptom might range widely in their level of discomfort. The evaluation starts with the question, "What do I see when I walk into the room?" like many other concerns in the ER. It's important to create a preliminary opinion within the first few seconds or minutes since you may need to act to stabilise the patient before you have enough data to make a definitive diagnosis.
Our first assessment of the patient is that she is in serious distress, has aberrant vital signs, and is breathing fast. We should be ready for an instant response.
Initial measures
It is very helpful to have extra assistance from nurses, doctors, or other ED professionals. When evaluating your patient's ABCs, you should concurrently request the following:
- A complete set of vital indicators, including BP, HR, RR, SpO2, and temperature
- Cardiac and pulse oximetry monitoring
- IV access, including blood draw for ABG/VBG and another routine testing
- In some circumstances, obtaining an electrocardiograph (ECG) may be helpful as well
- Oxygen application via nasal cannula, non-rebreather mask, or bag-valve-mask if the patient requires assisted ventilations (not breathing adequately on their own)
You may need to think about using more aggressive treatment methods like non-invasive positive pressure ventilation (NIPPV) or intubation if your patient does not react to oxygen delivery and is not breathing properly.
She is put on a non-rebreather mask at 15 LPM, but neither her distress level nor her oxygen saturation improves. The patient is put on the monitor after obtaining IV access. An electrocardiograph (ECG) reveals sinus tachycardia. She is able to keep her airway open and her mental state is fine. A BiPAP machine is called in to provide respiratory treatment.
Non-invasive ventilation: When to use it
|
Think about NIPPV for patients who have |
When NOT to use NIPPV |
|
|
History and physical evaluation
The history often offers hints as to the cause of your patient's symptoms, aiding in the development of a workable diagnosis. Ask the patient's relatives if they have any pertinent information if the patient is in respiratory distress and unable to speak. They can be knowledgeable of the patient's prior medical history or significant occasions that occurred before the patient's meeting. Medicines may be quite beneficial. For instance, someone using an albuterol inhaler is likely to have a history of COPD or asthma, while someone with a prescription for furosemide may have a history of heart failure.
Essential historical components:
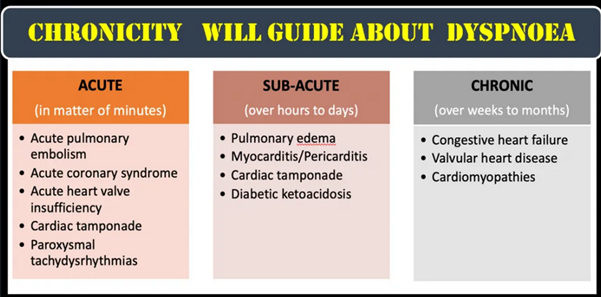
- Did the breathless start suddenly? If so, keep spontaneous pneumothorax or pulmonary embolism in mind. Slow development of symptoms is more indicative of congestive heart failure, pneumonia, or COPD.
- Is the breathlessness persistent or sporadic? Many chronic disease processes may sometimes become acutely worse. Your patient could even be able to describe how his or her symptoms resemble those of the most recent case of asthma, COPD, heart failure, pneumonia, etc.
- Is the breathlessness caused by effort or position? Orthopnea is often associated with CHF, although it may also be a sign of COPD, neuromuscular conditions, pleural/pericardial effusions, or ascites. Multiple factors, such as primary pulmonary illness, heart ischemia, or anaemia, may potentially contribute to exertional dyspnea.
- Did any precipitating events occur? Breathlessness that follows exposure to an environmental or known allergen might be a sign of an allergic response. Similar to a recent hospitalisation, extended travel might make you suspect PE.
- Does your patient's prior medical history mention anything important? As previously said, a history of conditions like asthma, COPD, or CHF might point to a possible explanation for your patient's symptoms. If your patient has a history of hypertension that was treated with an ACE inhibitor, there may be a greater risk that they may develop angioedema.
The physical examination may be quite beneficial in figuring out what's causing your patient's problems. Finding trends that support your history might help you do evaluations more effectively.
- An allergic reaction or angioedema may be indicated by visible oedema of the upper airway. Drooling, stridor, and altered voice are warning symptoms of imminent airway blockage and may be caused by an allergy, infection, or foreign substance.
- A pneumothorax, infectious consolidation, or effusion should be suspected when auscultation reveals focally absent or decreased breath sounds.
- Bronchospastic conditions including asthma, COPD, and anaphylaxis may cause wheezing.
- Pleural effusions, pneumonia, and PE may all cause rales. Rales may be a sign of CHF when present with peripheral oedema and JVD.
- Tenderness and swelling in one leg alone enhance the possibility of DVT/PE.
- Crepitus, bruising, and pain are indications of a pneumothorax, hemothorax, or pulmonary contusion, respectively.
- "Tripoding," or the employment of auxiliary muscles, may indicate imminent respiratory failure and the need for prompt treatment but may be less useful in diagnosing the cause.
The patient's attendants reported that our patient had stopped taking her prescriptions, which several number of antihypertensives and a diuretic, for a period of time. Upon physical examination, she was found to have raised JVP, pitting oedema in both legs and bilateral rales at the level of her shoulder blades. Her symptoms and vital signs start to get better when she is given nitroglycerin and put on BiPAP.
Evaluations for diagnosis
- Additional tests may be utilised to support a diagnosis or rule out other potentially fatal illnesses after the first evaluation and stabilisation of your patient.
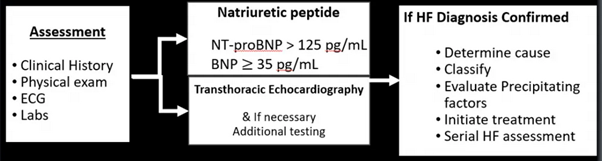
- Cardiac ischemia, dysrhythmia, PE, pericarditis, and pericardial effusion may all be detected with an EKG.
- In unstable patients, portable (bedside) AP views of the chest are often taken, while in patients who are stable and can be moved to radiology, PA/lateral views are frequently taken. They may show a variety of diseases, including pneumonia, pleural effusions, pneumothorax, and damage to the chest wall. Chest CTs may be used to check for aortic diseases, traumatic injuries, unusual infections, and pulmonary emboli.
- Compared to other methods, ultrasonography is often the quickest approach to obtaining more data. An ultrasound of the lungs may detect consolidation, pleural effusion, pulmonary oedema, and pneumothorax. Cardiac views may detect pericardial effusions, tamponades, and right heart strain, such as in PE or pulmonary hypertension, and left ventricular dysfunction, such as in CHF. Lower extremity DVTs are also evaluated with ultrasound.
- Laboratory testing may offer further details to a diagnosis or help with the workup (e.g., serial cardiac enzymes to rule out MI, d-dimer to rule out low likelihood PE, and BNP to check for CHF exacToIn order to ascertain a patient's actual oxygenation state, an ABG study may be required. Typically, a consistent waveform and a conventional SpO2 measurement are sufficient to assess the patient's oxygenation status.
- However, it could be challenging to get a dependable waveform in agitated, chilly, diaphoretic, or otherwise unreliable SpO2 individuals. To accurately calculate the oxygen partial pressure and saturation in this case, an ABG may be required. Accurate partial pressures of carbon dioxide will also be provided by the ABG. ABGs, on the other hand, must be obtained by an artery puncture and may not be as easily accessible as a VBG.
- Standard venipuncture during IV insertion may be used to collect VBGs. To calculate a patient's partial pressure of carbon dioxide, the VBG is essential. Tachypneic patients with elevated venous CO2 levels often have bronchospastic conditions, such as asthma or COPD. However, this can indicate inadequate overall ventilation in individuals with diminished respiratory drive.
Differential diagnosis
Patients with respiratory distress should be evaluated for the following critical diagnoses (and general treatment options):
- Anaphylaxis - Epinephrine, beta-agonists, antihistamines, steroids
- Acute coronary syndrome - Aspirin, antiplatelet agents, anticoagulation, reperfusion therapy
- Acute congestive heart failure exacerbation - Supplemental O2, PPV, nitrates, diuretics
- Asthma/COPD exacerbation - PPV, beta-agonists, steroids
- Cardiac tamponade - Pericardiocentesis
- Non-cardiogenic pulmonary edema - Supplemental O2, PPV, diuretics, antibiotics
- Pulmonary embolism - Anticoagulation, lytic agents (systemic or catheter-directed), thrombectomy
- Pneumonia - Antibiotics, supplemental O2, PPV
- Pneumothorax/tension pneumothorax - Needle decompression, tube thoracostomy
- Upper airway obstruction - Early intubation for airway protection (alternative: cricothyrotomy), treat the underlying cause
The physical examination is promptly followed by a bedside ultrasound. The ejection fraction of the heart is substantially reduced, and widespread B-lines indicative of pulmonary oedema are seen in the lung windows. Her symptoms and vital signs start to get better when she is given nitroglycerin and put on BiPAP.
Clinical examination: The first step in diagnosing heart failure
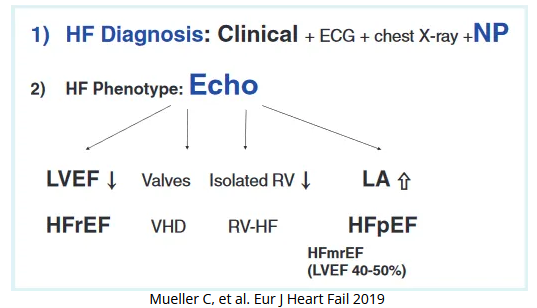
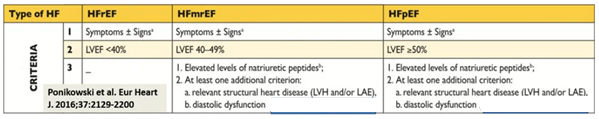
Latest HF categorisation
A greater understanding of how to treat HF
- The SGLT2i drugs dapagliflozin and empagliflozin are now included in the typical "quadruple therapy" that is recommended for all HFrEF patients, regardless of their diabetes status.
- (Mineralocorticoid receptor antagonist [MRA]) Empa/or DAPA, angiotensin-converting enzyme inhibitor [ACEi]/angiotensin neprilysin inhibitor [ARNi], and beta-blockers.
- In HF with a mildly reduced ejection fraction (HFmrEF), SGLT2i have a Class of Recommendation 2a. Beta-blockers, ARNi, ACEi, ARB, MRA, and other medications are given weaker recommendations (Class of Recommendation 2b) in this group.
Resolved case
With continued NIPPV and nitrate therapy, our patient's level of respiratory distress rapidly decreases, enabling her to avoid intubation. Following her hospital admission for an acute CHF exacerbation, she resumes taking her home medications. After several days of more diuresis, she feels normal again, so she returned home.
Key points
- Your first treatment strategy will be primarily determined by how well you evaluate the patient's work of breathing. Patients who are critically ill will need prompt therapy escalation, but it may be permissible to wait for diagnostic results before starting therapeutic treatments in patients who are less unwell.
- Bedside ultrasonography has developed into a potent diagnostic tool for acute dyspnea. Early in the treatment of the dyspneic patient, ultrasonography may be used to assist risk stratify patients for a variety of urgent reasons, such as acute heart failure exacerbation, pulmonary oedema, pleural effusion, pneumothorax, pericardial effusion, and pulmonary embolus.
- While family history may be useful in compiling information, resist the urge to base your diagnosis on information that may turn out to be inaccurate or otherwise irrelevant.
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr Monish Raut is a practising super specialist from New Delhi.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries