How I Managed an Emergency Case of Hypertension in ER: A Case Study
M3 India Newsdesk May 05, 2023
If untreated, hypertension can be deadly. Patients can run the danger of developing kidney failure, heart failure, or stroke. This article presents an interesting and detailed emergency case study of hypertension.
It was 6 pm and I finished my evening ICU rounds with my residents, I reached home and was in a relaxing mood because of the heavy workload in ICU. I slept early that day. Around 2 am received a call from my emergency physician about a patient relative of a renowned physician coming to the hospital in an unconscious state. By the time I reached the hospital patient was in ER with a history of receiving CPR in the car.
The case
This patient was 52 years old gentleman with known case of hypertension with c/o chest pain for 1 hour. He was pulseless, we immediately started cardiopulmonary resuscitation as per ACLS protocol. After around 30 minutes of continuous CPR, he was revived.
Diagnosis
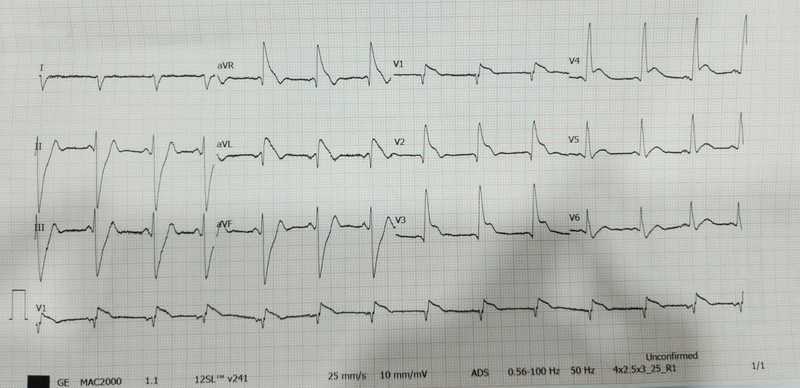
ECG was suggestive of changes in anterior wall myocardial infarction. The patient was intubated and put on a mechanical ventilator. The patient was loaded with dual antiplatelet, statin through Ryles tube and injection heparin as per protocol. The patient became conscious, the cardiologist was informed and the urgent need for primary angioplasty was discussed with relatives.
Treatment
The patient was in shock, so we started on Noradrenaline infusion; Arterial blood gas report was suggestive of severe metabolic acidosis which was treated with an injection of soda-bicarbonate. Cardiologist did bedside 2D-ECHO which was suggestive of Poor LV function with an Ejection fraction of 15% and anterior wall hypokinesia.
By the time patient reached the cath lab for emergency angioplasty patient again had cardiac arrest, ECG suggestive of ventricular tachycardia CPR was started on a cath lab table, DC shock of 200J given twice and the patient revived in 5-6 minutes, but the patient remained unconscious, we discussed with relatives about doubtful neurological status in view of prolonged CPR, being medico-family they immediately agreed for emergency angioplasty despite doubtful neurological status.
The patient underwent coronary angiography which was suggestive of single vessel disease with 100% thrombotic occlusion of the left anterior diagonal artery patient underwent primary angioplasty with stenting of LAD.
The patient was shifted to ICU around 4.30 am on vasopressors with a femoral arterial line. On neurological examination, the patient’s pupils were sluggishly reacting and there was no response to deep painful stimuli, he also had 1 episode of involuntary activity; seizures for which he was started on injection Levetiracetam.
Observation
- We started to post CPR care with a target temperature of 36’C. Over time patient’s blood reports arrived and his complete blood panel was normal his kidney function was deranged with a creatinine of 1.8mg/dl and his urea was 45mg/dl, his liver function test was in the normal range, and troponin I and CK-MB were high.
- Overnight patient’s hemodynamics remain stable and his vasopressors were tapered off.
- It was 8.30 am when I assessed the patient again and he was localising to painful stimuli we stopped hypothermia and started normalising his temperature.
- Around 10 am he had a very short episode of ventricular tachycardia which reverted without any medication repeat ECG had no fresh changes and 2D-ECHO was showing improving Ejection Fraction EF, so we continued same line of management, and repeat serum electrolytes were in the normal range.
- Till this time everyone was sceptical about the neurological status of the patient but around 11.30 am he started following simple verbal commands and moving all four limbs.
- Till evening he was on minimal vasopressors pouring a good amount of urine with a Glasgow Coma score of 15/15.
- The patient's ECG was showing sinus rhythm latest. The arterial blood gas report was normal; we decided to start weaning from the ventilator and he was put in a spontaneous mode which he tolerated well.
- Evening arterial blood gas was analysed and he was put on T piece with O2, looking at the patient's clinical progress and good ABG reports we planned for extubation on the next day.
Conclusion
This was an interesting and thrilling case in which a patient received multiple times CPR with doubtful neurological status who was diagnosed and treated with immediate and appropriate treatment and his life was saved that too with intact neurological status.
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr. Ramesh Hasani is an emergency care specialist at Seven Star Hospital, Nagpur.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries