Effective Evaluation Cervical Dysplasia Can Prevent Cancer
M3 India Newsdesk Feb 04, 2023
Cervical dysplasia is a precancerous disorder in which aberrant cell growth takes place on the surface lining of the cervix or endocervical canal, the entrance between the uterus and the vagina. The clinical management of this illness is covered in detail in this article.
Screening
A pap smear is the common screening test for early detection of cervical dysplasia. Liquid-based cytology now accounts for much cervical cytology testing as automated slide preparation and preliminary review are possible, and the remaining transport medium can be used for HPV and another testing.
Current guidelines recognise 3 effective ways for cervical cancer screening - cytology, co-testing, and primary HPV testing. Co-testing is cytology with a concurrent HPV test. Concurrent HPV negativity offers stronger reassurance that CIN 3+ is not present and will not develop over the next several years than cytology alone.

- Those over age 65 who have had regular screening in the past 10 years with normal results and no history of CIN2 or more serious diagnosis within the past 25 years should stop cervical cancer screening. Once stopped, it should not be started again.
- People who have had a total hysterectomy should stop screening unless the hysterectomy was done as a treatment for cervical cancer or serious pre-cancer. Those who had a supra-cervical hysterectomy should continue screening.
- People who have been vaccinated against HPV should still continue screening.
Based on the abnormality of the screening test, the next step in the evaluation may be colposcopy and biopsy. Cervical intraepithelial neoplasia (CIN) is a premalignant squamous lesion of the uterine cervix diagnosed by histologic examination.
Management
Age > 25
Cervical intraepithelial neoplasia (CIN) 1
1. Preceded by LSIL, ASC-US, or NILM but positive for HPV — low risk for the development of cervical cancer, and observation is therefore recommended with a one-year follow-up with HPV-based testing.
2. Preceded by ASC-H or HSIL — increased risk for subsequent high-grade disease.
- When preceded by HSIL cytology
An immediate diagnostic excisional procedure or observation (HPV testing and colposcopy at one year) is acceptable depending on the desire for future childbearing.
When observation is chosen:
- Colposcopy and HPV-based testing are performed for one year; if negative, then repeat HPV testing in one year.
- If HPV testing continues to be negative, then repeat HPV testing in three years, at which time long-term surveillance can begin.
- If any test is abnormal during observation, repeat colposcopy is recommended, and management is based on the biopsy result.
- If HSIL cytology is found at the one- or two-year visit, then a diagnostic excisional procedure is recommended.
- When preceded by ASC-H cytology
Observation is recommended provided the entire SCJ and lesion are visible on colposcopy and an ECC if collected, is negative. A diagnostic excisional procedure is not recommended.
HPV-based testing is performed for one year; if negative, then repeat HPV testing in one year.
- If HPV testing continues to be negative, then repeat HPV testing in three years, at which time long-term surveillance can begin.
- If any test is abnormal during observation, repeat colposcopy is recommended, and management is based on the biopsy result.
- If HSIL cytology is found at the one- or two-year visit, or if ASC-H is persistent at the two-year visit, then a diagnostic excisional procedure is recommended.
Cervical intraepithelial neoplasia (CIN) 2,3
1. If histologic HSIL is unspecified without distinction of CIN 2 or CIN 3:
- Treatment is preferred, and patients are managed as if CIN 3 were present.
- Observation (with colposcopy and HPV testing at 6 and 12 months) is acceptable.
2. If CIN 2 is specified:
- Treatment is recommended.
- Observation (with colposcopy and HPV testing at 6 and 12 months for up to two years) is acceptable if the entire SCJ and lesion are visible on colposcopy, and ECC does not demonstrate CIN 2+ or ungraded CIN after getting informed consent.
3. If CIN 3 is specified, if the entire SCJ or lesion are not visible on colposcopy, or if the ECC is CIN 2+:
- Treatment is recommended.
- Observation is unacceptable.
When treatment is planned, a diagnostic excisional procedure (LEEP, cold knife cone, and laser cone biopsy) is preferred. An ablation (with cryotherapy, laser ablation, and thermablation) is an acceptable alternative.
Hysterectomy is not acceptable for the primary treatment of HSIL (CIN 2 or 3).
Age < 25
Cervical intraepithelial neoplasia (CIN) 1
1. Preceded by LSIL or less
Cytology should be performed in one year.
If cytology is LSIL or less, cytology should be repeated in one year.
- If NILM, routine screening (with cytology when <25 years, and with human papillomavirus-based testing when ≥25 years) can resume.
- If ASC-US or greater, colposcopy should be performed.
If cytology is HSIL or greater, colposcopy should be performed.
2. Preceded by ASC-H or HSIL
- If the preceding cytology was HSIL, then observation consists of colposcopy and cytology in one and two years.
- If the preceding cytology was atypical squamous cells that cannot exclude HSIL (ASC-H), then observation consists of cytology alone in one and two years.
- If during observation high-grade cytology (ASC-H or HSIL) persists for two years in the absence of a histologic HSIL, then a diagnostic excisional procedure is recommended.
A diagnostic excisional procedure is recommended if the entire SCJ or lesion is not visible on the colposcopy.
Cervical intraepithelial neoplasia (CIN) 2,3
If histologic HSIL is unspecified. Observation or treatment is acceptable.
1. If CIN 2 is specified:
- Observation is preferred.
- Treatment is an acceptable option.
2. If CIN 3 is specified or if the entire SCJ or lesion is not visible on colposcopy:
- Treatment is recommended.
- Observation is unacceptable.
When observation is performed:
- Observation should initially consist of cytology and colposcopy at 6 and 12 months.
- If cytology is less than ASC-H and histology is less than CIN 2, then subsequent testing should occur in one year.
- If CIN 2 or unspecified HSIL persists for more than two years, then treatment is recommended.
When treatment is planned, a diagnostic excisional procedure is performed; ablation is an acceptable alternative.
Prevention
- Three HPV vaccines—9-valent HPV vaccine (Gardasil 9, protects against nine HPV types 6, 11, 16, 18, 31, 33, 45, 52, and 58), quadrivalent HPV vaccine (Gardasil,), and bivalent HPV vaccine (Cervarix). All three protect against HPV types 16 and 18 which cause most HPV cancers.
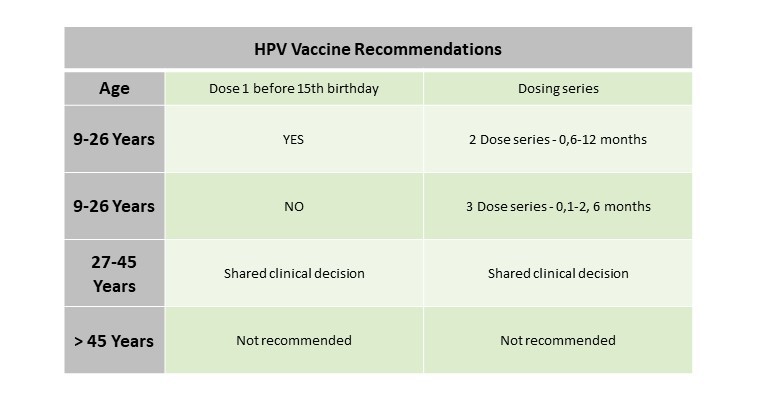
- HPV vaccination is recommended for ages 11–12 years. Can be given starting at age 9 years.
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr Amrutha C.V. is a practising gynaecologist from Kochi.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries