Emerging Concerns of Polypharmacy
M3 India Newsdesk Apr 19, 2023
Polypharmacy refers to using 5 or more medications based on a review of current data. This article explains the adverse effects of polypharmacy and its prevention along with case studies.
Polypharmacy
Polypharmacy, in modern scenario is almost inevitable (unless one is extremely healthy) ; but a health-practitioner should always assess the potential benefits as well as side effects while prescribing multiple drugs.The cutoff point of 5 drugs is associated with the risk of adverse outcome such as falls, frailty, disability and mortality in older adults as depicted in the Concord Health and Aging Men project.
As multimorbidity (coexisting of 2 or more chronic health conditions) is related to aging population, so polypharmacy and old age are almost synonymous. Though older person consume almost half of the total drug expenditure, they have a significant higher disease burden compared to younger adults.
The World Health Organisation suggest that while the definition is numerical, emphasis should be on evidence based practice and the goal of reducing in inappropriate polypharmacy.
Appropriate polypharmacy - When all medicines are prescribed to achieve the specific therapeutic objective and medication therapy has been optimised to prevent adverse drug reaction.
Inappropriate polypharmacy - It is usually called conventional polypharmacy, when one or more medications are prescribed (in addition to the specific medicines) than clinically indicated resulting in adverse patient outcome and not achieving therapeutic objective.
It may be due to patient related or doctor related.
A. Patient related - Taking herbal medicines or OTC medicines without doctor’s advice in addition to prescribed medicines.
B. Doctor related -
- Narrow focus on specialty (unaware of the best treatment of other medical conditions).
- Not aware of age associated side effects and drug interactions.
- Prescribing inappropriate medicines without referring to concerned specialist doctors.
- Poor communication with patients regarding prescription.
- OTC and herbal preparation.
- Excess drug prescription due to:
- Lack of morality
- Hyposkilliac
- Corporate hospital pressure
To summarise, it could no longer be assumed that polypharmacy is always harmful. The clinical reasoning in which the medicines have been prescribed needs to be considered. Appropriate and targeted drug therapy for disease management should be the goal.
Physiological changes in geriatric age group (related to pharmacokinetics)
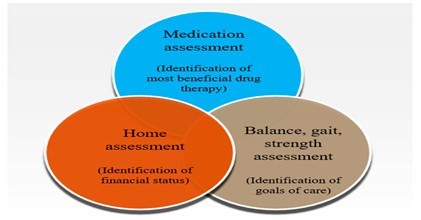
- As polypharmacy is related to old age, we should know the physiological changes related to old age and the pharmacokinetics (absorption, distribution, metabolism and elimination of drugs) and pharmacodynamics (end organ effects related to drugs) of geriatric age group.
- After 50 years, due to reduction in liver mass & reduction in hepatic blood flow, flow dependent clearance of drugs like verapamil, lidocaine, labetalol are decreased.
- Majority of the drugs or their metabolites are excreted by kidney. Other routes of elimination are liver, bile, gut, lungs.
- Glomerular filtration, active secretion by proximal tubule, passive reabsorption of kidney tubules are the main route of excretion Clinically, eGFR is preferred to monitor kidney functions (though mGFR-measured GFR is the gold standard) which is usually decreased in old age.
<30% decline in pharmacokinetic parameter usually does not need dose modification ; >=50% reduction in renal excretion needs maintenance dose adjustment (dose reduction, interval prolongation or both). Moreover associated co-morbid CKD patients also have hepatic and biliary dysfunction through which the drugs are excreted.
- In old age, associated hypoalbuminaemia increases the free drug and may result in toxicity. Alteration of renal blood flow and urinary pH also affect the renal excretion of drugs.
Concerns of polypharmacy
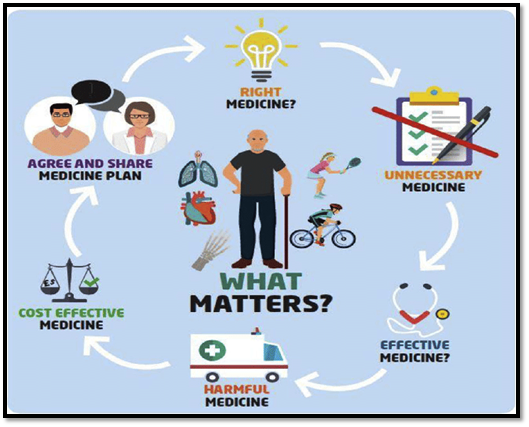
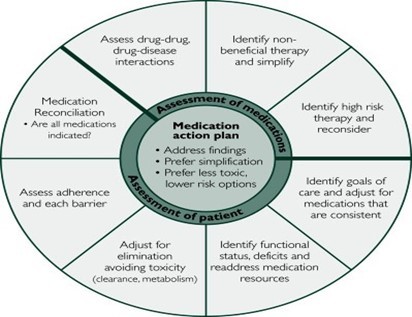
While prescribing multiple drugs in a patient, we should be rational first. We should ask ourselves;
- Are all medicines (at the said dose) required for the patient?
- Can using multiple medicine aggravate the condition or bring other drug related toxicity ?
- Can any medicine be deprescribed?
We have to make a balance between potential benefits and their side effects.
The concerns of polypharmacy are described as follows:-
1. Non Adherence- Due to multiple medication, as a result of visual and cognitive decline in old age, resulting in treatment failure and / or hospitalisation. Medication safety review clinic Taiwan study- 34% were non adherent with >25% of medicines.
2. Due to cost- In a poor country like India, this is the most common cause.
3. Adverse drug effect- An adverse drug reaction refers to the harm caused by a drug at usual doses. 5-28% of acute geriatric medical admissions are due to ADE. The drug classes commonly associated with preventable ADE are cardiovascular drugs, anticoagulants, diuretics, hypoglycemic and NSAIDs. This is due to metabolic changes and decrease drug clearance that comes with age. The risk increases by increasing the no. of drugs used.
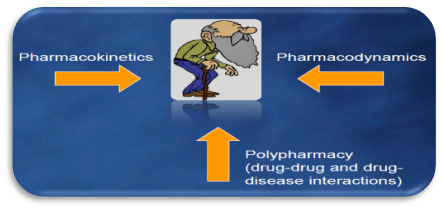
4. Potential drug - drug interaction per patient- A drug-drug interaction refers to the pharmacological or clinical response to the administration of a drug combination that differs from the response expected from the known effects of each of these two agents when given alone. The most common adverse drug interactions related adverse events are neuro –psychological (delirium), acute ARF and hypotension.
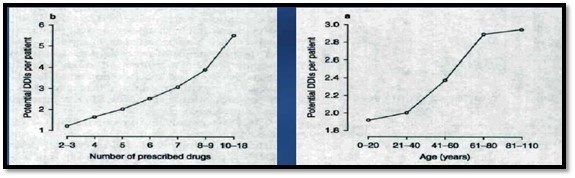
[ Retrospective results from 81,650 outpatients at a Taiwanese medical center between January and March, 2004. Included patients had 2+ prescriptions and had used each drug for at least 14 days]
5. Risk of hip fracture- Polypharmacy has shown increase risk of hip fracture in older adults in some case control study.
6. Prescribing cascades- Polypharmacy increases the possibility of prescribing cascade , when additional drugs are prescribed to treat other drugs’ adverse effects by misinterpretation of ADE as new medical condition. One example given is as follows;
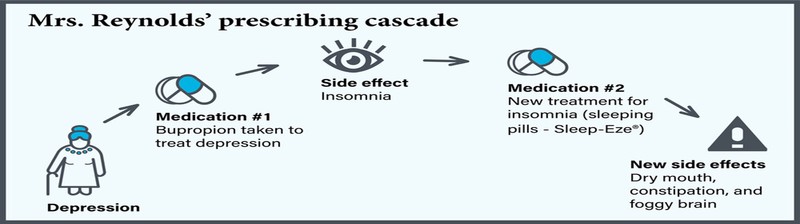
Adding drugs to treat drug side-effects
- Justifiable examples
- Laxatives for opioid- induced constipation.
- Antacid to reduce risk of gastritis during NSAID administration.
- Probably not justifiable examples
- An anti-psychotic medicine prescribed for hallucinations in patient taking ropinirole (Requip) for restless leg syndrome. A side-effect of Requip is hallucinations.
- The anti-incontinence drug, oxybutynin, prescribed for night time incontinence in patient taking a diuretic at bedtime.
Case studies
Case study 1
A 70 year old obese female , who is a known case of diabetes, hypertension, LV diastolic dysfunction, dyslipidemia ; with sensory neuropathy, eGFR - 42, glaucoma, depression, had visited primary doctor and then subsequently to different specialist. The medicines taken by her currently are as follows:
- Metformin (1000 mg) - 1 tab BD
- Gliclazide 80 - 1 tab BD
- Metoprolol 50 - 1 tab OD
- Torsemide 40 - 1 tab OD
- Telmisartan 80 - 1 tab OD
- Atorvastatin 40 - 1 tab OD
- Amitriptyline 25 - 1 tab HS
- Duloxetine 20 - 1 tab OD
- Clonazepam .5 - 1 tab HS
- Gabapentin 300 - 1 tab TDS
- Timolol .5 - 1 drop for both eyes daily
- Ranitidine 150 – 1 tab BD
- (OTC) Antihistaminic at bedtime for sneezing
Are these medications rational / appropriate?
- eGFR - 42, She is G3b category CKD. So, dose of metformin to be reduced.
- Amitryptyline , Clonazepam and Antihistaminic can cause confusion.
- Metoprolol ( for high BP ) plus Timolol for glaucoma.
- Timolol has an additive effect with Metoprolol which can lower heart rate and BP.
Case study 2
A 75 year male who is a known case of diabetes, hypertension with LV dysfunction (ejection fraction 45%), had presented with hemorrhagic CVA, was discharged with following medications after treatment in the hospital:
- Inj Ryzodeg (Degludec/Insulin Aspart) - 10 IU at morning, 6 IU at evening
- Glimepride+Metformin (2/1000) - 1 tab OD
- Tab Pioglitazone(15 mg) – 1 tab OD
- Tab Phenytoin 100 - 1 tab TDS
- Tab Clonazep (.5) - 1 tab HS
- Tab Amitryptyline (10 mg) - 1 tab HS
- Tab Telmisartan + Cilnedipine – 1 tab OD
- Tab Torsemide 10 – 1 tab OD
- Tab Metoprolol 25 – 1 tab OD
Are these medications rational / appropriate?
- Glimepride +Metformin- long acting Sulfonylurea to be avoided in old age and better to be replaced with gliclazide or glipizide. Moreover dose of metformin may be reduced after assessing the kidney status.
- Pioglitazone to be omitted in LV dysfunction. Voglibose can be added if PPG is high.
- Phenytoin is usually not advised after 60 yrs (ataxia is a side effect of phenytoin). If AED is required levetiracetam or lamotrigine is to be added.
- Amytriptyline and clonazepam not to be added in old age as it can cause confusion and much sedation.
- Regular electrolyte and KFT function test is required in this patient.
Take home messages
- Polypharmacy can increases the risks of adverse drug reactions (ADRs). It can also play an important part of the optimal treatment of medical conditions. Goal is SMART prescribing.
- Minimise the number of potentially inappropriate medications (PIMs). [Beers criteria comes in handy.( The Beers Criteria presents a list of medications where the risk of harm outweighs potential benefits (American Geriatrics Society, 2018). It also lists high-risk drug–drug interactions to avoid and identifies agents requiring renal dosing adjustments (American Geriatrics Society, 2018).
- The integration of STOPP (Screening Tool of Older Person’s Prescriptions) and START (Screening Tool to Alert to Right Treatment) for medication review in multi-morbid older people can be practiced in clinical setting.
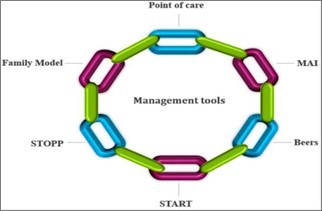
- Try to start a new medication at the lowest dose and then titrate slowly. Exercise careful medical reconciliation during transitions of care and provide proper communication handoffs to accepting providers.
- Always ensure a post discharge follow up for updating medical history and medications. This can help in preventing medication errors, treatment failures and re-hospitalisations. Encourage patients to bring all medications, including prescriptions, OTC, supplements and herbal preparations during follow up visits.
- Use a team approach, if possible, involving every level healthcare worker, family members and (community) pharmacist. Holistic, shared decision making conversations should become part of routine practice.
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr Samir Kanti Datta is a practising physician from West Bengal.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries