Downs Syndrome: Clinical & Oral Features and Dental Management
M3 India Newsdesk Jan 31, 2025
Down's syndrome (DS or DNS), also known as trisomy 21, is a genetic disorder caused by the presence of all or part of a third copy of chromosome 21. This article presents the clinical manifestations and dental management of oral diseases in individuals with Down's Syndrome.
Down's syndrome
Down's syndrome is named after John Langdon Down, the British doctor who first described the condition in 1887. The incidence is reported to be 1 in 600 t births; however, more than half of the affected foetuses spontaneously abort during early pregnancy.
Like most trisomies, the incidence of trisomy 21 is highly correlated with maternal age, increasing from about 1/1500 live births for women 20 years of age to 1/30 for women 45 years of age and older. Prenatal diagnosis is possible via amniocentesis, chorionic villus sampling, or percutaneous umbilical blood sampling.
Because these tests are invasive, an individualised risk assessment based on maternal age, maternal serum markers (e.g., serum alpha-foetoprotein), and foetal physical markers (e.g., nuchal translucency on ultrasonography) may be carried out to identify elevated risk and the requirement for additional testing.
DS is typically suspected and diagnosed at birth based on clinical symptoms and cytogenetic investigations, respectively, if it is not identified during pregnancy.
Clinical presentation and characteristic features
- Learning disability (100%), is the most frequent genetic cause of mild to moderate learning disability.
- The most common features among DS patients include short stature, brachycephaly (small head), rounded small face, mid-face hypoplasia with a flat nasal bridge, the upward slant of the eyes (slanted palpebral fissures) and epicanthic folds.
Oral features of Down's Syndrome individuals
1. Tongue and lips
- DS individuals ' common oral soft tissue features include large, fissured tongues and cracked lips.
- Generalised hypotonia of the orofacial muscles, e.g., the orbicularis, zygomatic, masseter, and temporalis muscles, enhances improper oral seal, poor suckling, poor tongue control, and jaw instability.
- Persistent mouth opening due to the relatively large tongue in a reduced oral cavity may lead to mouth breathing, drooling, chapped lower lip and angular cheilitis.
- Since they verified a decreased stimulated parotid salivary flow rate, it was claimed that DS patients' drooling was caused by open mouth posture, a protruding tongue, and hypotonic orofacial muscles rather than hyper-salivation.
- This population has also reported an increase in bifid uvula, submucous cleft and cleft palates.
2. Mid-facial complex and palate
- The development of the whole craniofacial complex is retarded and the facial profile is relatively concave.
- The maxilla is deficient in development while the mandible is of normal size or slightly hypoplastic. The deficiency in the vertical height of the maxilla results in the overclosure of the mandible and thus projects the lower arch forward relative to the upper.
- Such patients show a significantly higher frequency of shelf-like or "stair palate".
3. Occlusion
- Malocclusion is a common finding in DS individuals.
- Malocclusion is influenced by the following factors: dental agenesis, delayed eruption, characteristic tongue push, anterior open bite, tooth spacing, and/or exfoliation of the permanent and deciduous dentition, midline deviation in upper arch, mouth breathing, improper chewing, bruxism, dysfunction of temporomandibular joint (TMJ), hypotonic ligamentary apparatus of TMJ, developmental disturbances of the mandible (platybasia) and maxilla (mid-facial complex) and the jaw relationships.
- Angle Class III malocclusion was present in two-thirds of DS individuals. The higher incidence of Class III malocclusion is due to under-development of the midface and not due to prognathism.
4. Tooth
- DS individuals presented with true generalised microdontia in permanent dentition, but in primary dentition, this is not well documented.
- Clinical crowns are frequently conical, short and small.
- They examined the lower incisors' dimensions and found that the reduced permanent crown size was linked with a reduction in both enamel and dentine thickness.
- It was reported that all teeth except the upper first molars and lower incisors were reduced in size, with complete root formation.
- Peg-shaped lateral incisors, shovel incisors and slender canines were frequently seen.
- Enamel hypoplasia and hypocalcification, affecting both primary and permanent dentitions are relatively common in DS children.
- The crown and root lengths of permanent teeth are shorter than usual, with the exception of the mandibular first premolar.
- Taurodontism is a frequent finding in persons with DS. When combined with abnormally short roots, taurodontism would lessen the amount of periodontal attachment and cause the tooth movement that these people frequently experience.
Oral diseases in individuals with Down's Syndrome
1. Dental caries
- The low prevalence of dental caries in both primary and permanent dentitions of DS individuals has been widely reported.
- Young DS children have feeding problems or behavioural difficulties and are hence dependent on bottle feeding for a prolonged period, thus increasing the risk of nursing bottle caries.
- Caries-free DS patients reported higher salivary-specific IgA concentrations but much lower Streptococcus mutans numbers.
- The low caries prevalence is anticipated to be due to delayed eruption, reduced time of exposure to a cariogenic environment, microdontia, spaced dentition, congenitally missing teeth, shallow fissures of the teeth, higher salivary pH and bicarbonate levels.
2. Periodontal disease
- DS individuals usually present with poor oral hygiene, expressed as marginal gingival inflammation, acute and subacute necrotising gingivitis, gingival recession, increased pocket depth, advanced chronic periodontitis, alveolar bone loss, suppuration or even abscesses, furcation involvement, increased tooth mobility, and even tooth loss.
- DS individuals had a prevalence of 60 to 90% and increased severity of periodontal disease as compared to age-matched normal controls and subjects with other mental disabilities.
- The severity of periodontal disease was investigated in DS individuals as compared to healthy individuals or cerebral palsy patients. According to their findings, DS patients had noticeably greater levels of periodontal inflammation and treatment requirements.
Dental management
1. Risk assessment
- In general, it is mandatory to check a patient’s medical and dental history and to do a comprehensive assessment. Infection control and aggressive elimination of any dental infection are important.
- Also, assessment regarding drug use for cardiac defects (e.g. platelet aggregation inhibitors) and making sure that the patient receives proper medical care.
- Consultation with the patient’s health care provider is recommended before commencing dental treatment.
2. Cooperation
- Children with DS have learning disability but exhibit a wide range of behaviours in the dental setting, including cooperation, compliance, mild to moderate anxiety, phobia and complete lack of cooperation.
- For many patients, it is possible to carry out simple restorative treatment and preventive measures using standard behavioural management techniques such as tell-show-do, positive reinforcement, modelling, distraction and both verbal and nonverbal communication.
- Also, it is recommended to keep the appointment short and focus on a specific treatment.
3. Parents and caregivers' oral health education
Good oral hygiene is the responsibility of the primary caregiver until the individual can develop the necessary coordination to become self-sufficient.
4. Local anesthesia
Most DS patients can be treated under local anaesthesia with awareness of patient positioning to avoid neck hyperextension.
5. Conscious sedation
Can be very useful to reduce anxiety, although careful assessment of respiratory function and infection is important. There may be complications of airway management due to a short neck, large tongue obstructed nasal passage and sleep apnoea.
6. General anesthesia
- Children with DS exhibit Atlanto axial joint instability (AAI) and extreme care is needed during intubation and orientation of the head by the paediatric dentist during the provision of dental treatment under general anaesthesia.
- It is also difficult to do endotracheal intubations due to a large protuberant tongue, high-arched palate, small mouth, short, broad neck, abnormal dentition, small maxilla & mandible, and large tonsils.
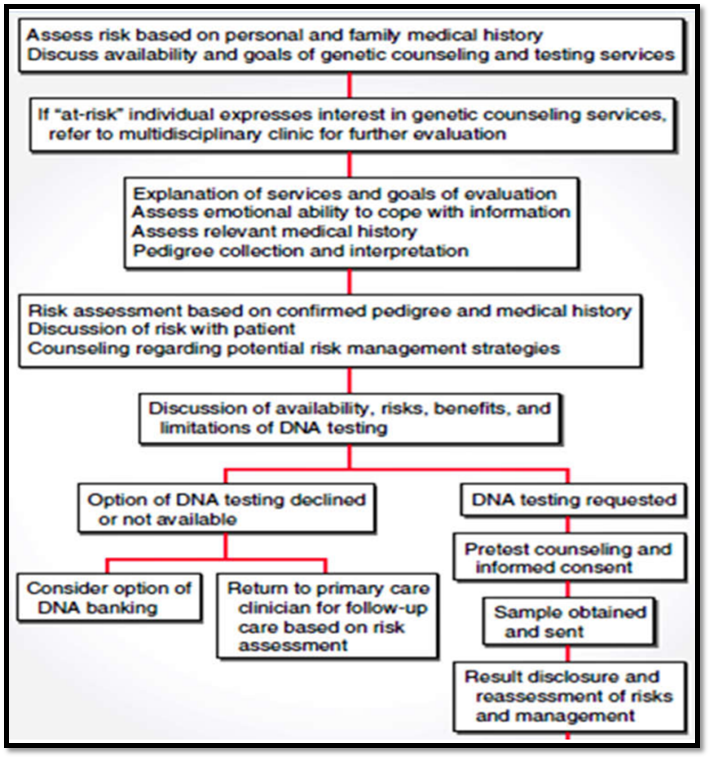
7. Genetic counselling
- Genetic counselling must be given to married couples to prevent consanguineous marriages.
- The chart given below has the protocol to be followed.
Takehome message
- Down’s Syndrome individuals are a group of patients requiring special oral health care services.
- They have more orodental issues and are often affected by malocclusion. The dental care must be provided with special dental care services for this population, as they are unmet.
- DS care providers should acquire an appropriate level of oral health awareness and communities and consider improving the accessibility of DS subjects to oral health care to assist maintenance of oral and overall health for this group of special needs patients.
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr Neha Kalantri is a practising dentist from Nashik.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries