Disease Patterns of Juvenile Dermatomyositis
M3 India Newsdesk Jun 22, 2023
Juvenile dermatomyositis (JDM) is a rare autoimmune disease in children that causes muscle weakness and skin rashes. This article explains how early recognition and treatment are crucial to minimise complications and improve outcomes in JDM.
Case presentations on juvenile dermatomyositis
Case 1
A 12-year-old girl presented with muscle weakness especially involving proximal muscles with a history of inability to comb hairs, difficulty climbing stairs and getting out of bed and skin rash.
Diagnosis: She was diagnosed with JDM and treated with steroids and immunosuppressive medications, which improved her symptoms. However, she experienced multiple disease flares over the next few years, with worsening muscle weakness and skin rash.
She required several hospitalisations and changes in medications to control her disease. Later on, she also developed Lipodystrophy and calcinosis.
Case 2
A 10-year-old boy also presented with proximal muscle weakness and skin rash-like bluish discolouration around the eyelid, nodules over interphalangeal joints and erythema involving the nasolabial fold.
Diagnosis: He was diagnosed with JDM and treated with steroids and immunosuppressive medications, which quickly resolved his symptoms. He remained in remission for several years, with no further disease activity or need for medications.
These two case reports illustrate the different disease patterns seen in JDM.
The disease pattern of JDM is highly variable and can range from mild to severe, with different degrees of muscle and skin involvement. Some patients may have a single episode of the disease, while others may experience frequent flares and require ongoing treatment. Early recognition and treatment of JDM are important to minimise long-term complications and improve outcomes.
Juvenile dermatomyositis (JDM)
Juvenile dermatomyositis (JDM) is a rare autoimmune disease characterised by proximal muscle weakness and the presence of characteristic rashes.
The incidence of this condition is about 3.2 cases per million children per year.
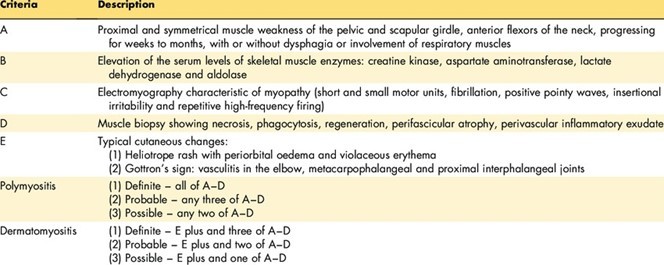
It is the inflammation of capillaries characteristically involving the skin and muscle as the name would suggest. However, any organ can be involved in this condition. Bohan and Peter put forward diagnostic criteria for the diagnosis of adult as well as juvenile dermatomyositis.
Bohan & Peter criteria for dermatomyositis:
Amyopathic JDM (dermatomyositis sine myositis)
Some children are present with classic rash but no apparent muscle inflammation or weakness.
Depending on how the disease progresses in the first two years, the course of the illness may be monocyclic, polycyclic, or chronic continuous.
Disease course
On the basis of the pattern of their disease patients were categorised to have the following disease course:
- If a patient reached clinical remission, as shown by a lack of disease activity by clinical and laboratory examination, within two years of the disease beginning, the patient was said to have a monocyclic course.
- Polycyclic if there is a recurrence of disease activity after a definite. remission as chronic continuous if the disease is active without remission even after 2 years of diagnosis,
- Undefined if less than 2 years of follow-up is available after diagnosis.
Disease characteristics
-
The mean age at the onset of the disease was 7.74 ± 3.74 years.
- The male-to-female ratio was 1:2. The mean duration of time from the time of onset of symptoms to diagnosis was 2.5 months (range 2 weeks 1 year).
- The duration of follow-up ranged from 11 months to 6.8 years with a mean of 2.87 ± 2.23 years.
Clinical Features
Skin Rash
- Erythema over neck and chest - Shawl sign
- Blue-violet discolouration of the eyelid - Heliotrope Rash
- Bright pink shiny or pale, thickened or atrophic papules over Interphalangeal joints - Gottron Papules
- Thickened erythematosus and scaly rash over palm - Mechanics hand
- Muscle involvement- Insidious in onset
- Typically symmetrical, affecting proximal muscles such as neck flexors, shoulder girdle and hip flexors
(Gower sign - Use of hand on thighs to stand from a sitting position)


Heliotrope rash

Gottron papule
Clinical features
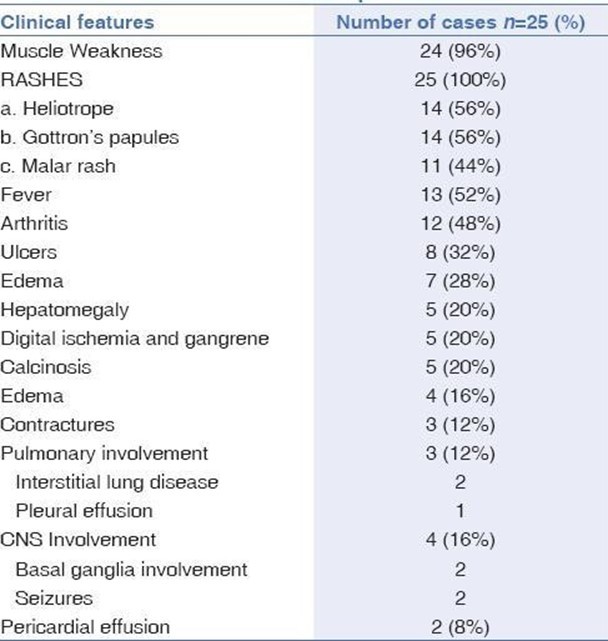
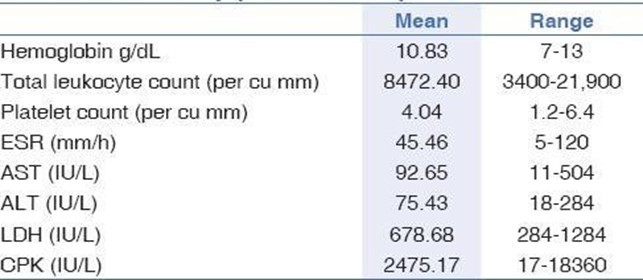
Laboratory features
Differentiating features from adult dermatomyositis
- Unlike adult DM there does not seem to be an increased risk of malignancy in JDM.
- Calcinosis, which is relatively rare in adults, is found in 6–50% of children with JDM.
- Acquired lipodystrophy, a rarely reported feature in adult DM, is a relatively common finding in patients with JDM occurring in the region of 10% of children.
- Antibody frequency and phenotype association differ somewhat between adult DM and JDM. For example, anti‐Jo‐1 occurs in around 20% of adult myositis cases but occurs in only a few per cent of JDM patients. Anti‐TIF‐1γ is associated with cancer in adult disease; whereas in juvenile disease there is an association with ulcerating skin lesions.
Management
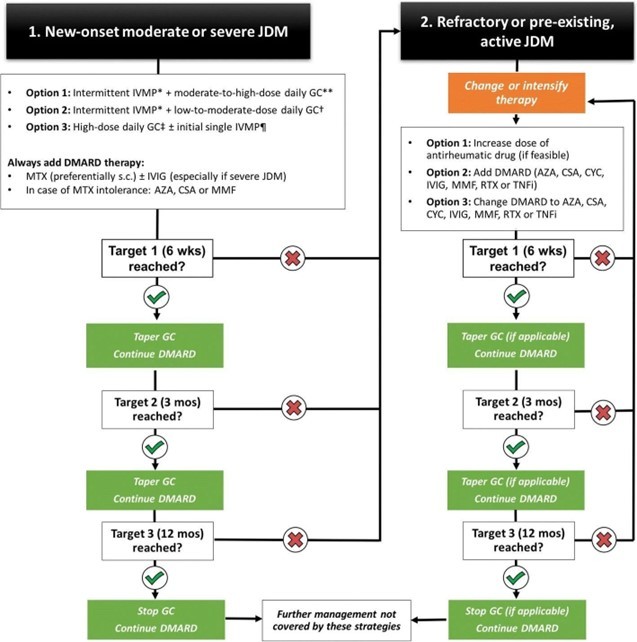
- IVMP - 30mg/kg/day
- GC - 1.5-2 mg/kg/day
- Methotrexate - 15-25 mg/m2/wk
Conclusions
- JDM, though rare should always be considered in the differential diagnosis of any child with skin rash and muscle weakness.
- Monophasic disease seems to be the commonest disease course in our cohort.
- When diagnosed early and treated appropriately, sustained remission without medications is possible in a good proportion of patients.
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr Monica Gundecha is an MD (skin & VD) from Pune.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries