Dealing with the Candida Infections: IDSA Recommendations
M3 India Newsdesk Nov 03, 2017
In India, 270,284 hospital admissions per year are attributed to Candida related infections, which also means that 21.1 per 100,000 people suffer from Candida infection.
The Infectious Diseases Society of America (IDSA) issued a revised guideline, endorsed by American Academy of Pediatrics (AAP), the Pediatric Infectious Diseases Society (PIDS), and the Mycoses Study Group (MSG), for the treatment and management of Candida infections.
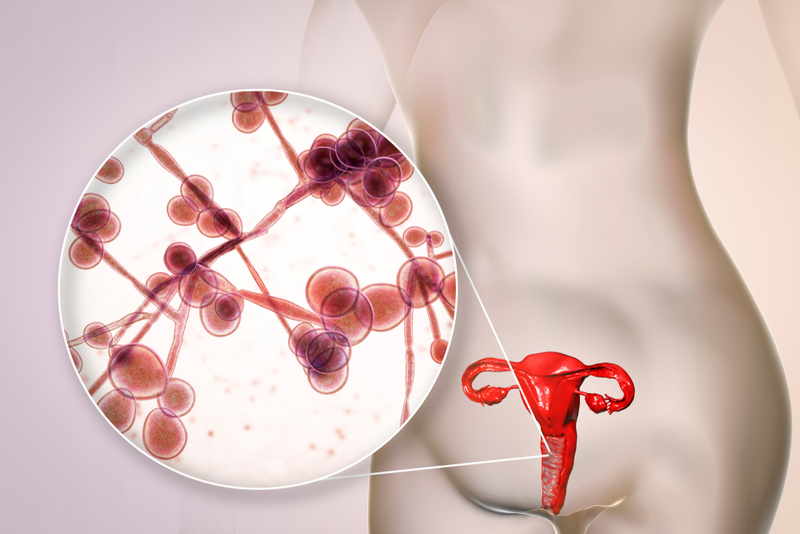
Although there are about 15 species of Candida known to cause infections in humans, the five most common pathogens that cause more than 90% of invasive diseases are C.albicans, C.glabrata, C.tropicalis, C.parapsilosis, and C.krusei. The infections caused by these organisms are collectively termed as ‘invasive candidiasis’, though each organism is unique in its epidemiology, virulence potential, and antifungal susceptibility.
Below mentioned are the strong treatment recommendations for different types of Candida infections:
Treatment for Candidemia in Nonneutropenic Patients
An echinocandin may be used in initial therapy; an alternative to echinocandin is fluconazole which can be used in patients who are not critically ill and are less-likely to have fluconazole-resistant Candida sps. Azole susceptibility testing for all blood-stream and echinocandin susceptibility testing is recommended in patients treated with echinocandin in the past and patients infected with C.glabrata and C.parapsilosi.
In case of intolerance, limited availability, or resistance to other antifungal agents, a reasonable alternative is lipid formulation amphotericin B (AmB. Transition to fluconazole from AmB after 5-7 days is recommended in clinically stable patients, who have isolates that are susceptible to fluconazole and in whom repeat cultures on antifungal therapy is negative.
A dilated ophthalmological examination needs to be done by an ophthalmologist within the first week of diagnosis of candidemia for all nonneutropenic patients. Blood culture should be repeated frequently, every 24 or 48 hours, to establish the time-point of clearance of candidemia.
Removal of Central Venous Catheters in Nonneutropenic Patients
Central Venous Catheters (CVCs) should be removed at the earliest in the course of candidemia when the source is presumed to be the CVC.
Treatment for Candidemia in Neutropenic Patients
An echinocandin may be used in initial therapy. Duration of therapy, without metastatic complications, is 2 weeks. Therapy is considered to be complete with documented clearance of Candida sps from the blood stream and resolution of neutropenia and candidemia symptoms.
Treatment for Chronic Disseminated (Hepatosplenic) Candidiasis
Lipid formulation AmB or an echinocandin may be used in initial therapy for several weeks followed by oral daily, for patients who are unlikely to have a fluconazole-resistant isolate. Infection may recur on premature discontinuation of antifungal therapy. Therefore, therapy should be continued until lesions resolve on repeat imaging, which usually takes several months.
Empiric Treatment for Suspected Invasive Candidiasis in Nonneutropenic Patients in ICU
Empiric antifungal therapy is recommended for critically ill patients with risk factors exclusively indicating invasive candidiasis and should be based on clinical assessment of risk factors, surrogate markers, and/or culture data from non-sterile sites. Therapy should be initiated as soon as the patient is diagnosed with risk factors and show clinical signs of septic shock.
Treatment for Neonatal Candidiasis, Including Central Nervous System (CNS) Infection
For neonates with disseminated candidiasis, AmB deoxycholate (1mg/kg daily) may be used. Preferable alternative in patients who have not been on fluconazole prophylaxis is fluconazole.
Treatment for Intra-abdominal Candidiasis
For patients with clinical evidence of intra-abdominal infection, empiric antifungal therapy may be used. The adequacy of source control and the clinical response would determine the duration of therapy.
Treatment for Candida Intra vascular Infections, including Endocarditis and Infections of implantable Cardiac Devices
1. Endocarditis is treated with lipid formulation AmB, with or without flucytosine, or high-dose echinocandin. A minimum of 6 weeks of treatment should be followed after surgery or for a longer duration in patients with perivalvular abscesses and other complications. Valve replacement is recommended. For patients who cannot undergo valve replacement, long term suppression with fluconazole may be followed.
2. The entire device should be removed in pacemaker and implantable cardiac defibrillator infections. Antifungal therapy is the same as that recommended for native valve endocarditis.
3. Suppurative Thrombophlebitis may need removal of catheter and incision and drainage or resection of the vein followed by intensive antifungal therapy.
Treatment for Candida Osteoarticular Infections
Osteomyelitis os treated with fluconazole or an for at least 2 weeks followed by fluconazole for 6–12 months. Surgical debridement is recommended in selected cases
Treatment for Candida Endophthalmitis
Within the first week of therapy in nonneutropenic patients, to confirm the presence of endophthalmitis, all patients with candidemia should have a dilated renal examination. For neutropenic patients, examination may be delayed till neutrophil recovery. Only an ophthalmologist should determine the extent of ocular infection. An ophthalmologist and an infectious diseases physician should collectively decide the antifungal treatment and surgical intervention
Treatment for Central Nervous System (CNS) Candidiasis
Liposomal AmB with or without oral flucytosine, may be used in initial therapy. Therapy should continue until all signs and symptoms, and CSF and radiological abnormalities have resolved. Infected CNS devices, including ventriculostomy drains, shunts, stimulators, prosthetic reconstructive devices, and biopolymer wafers that deliver chemotherapy should be removed.
Treatment for Urinary Tract Infections Caused By Candida sps
feasible, elimination of predisposing factors, such as indwelling bladder catheter should be considered. Treatment with antifungal agents is NOT recommended unless the patient belongs to a group at high risk for dissemination; high-risk patients include neutropenic patients, very-low-birth-weight infants (<1500 g), and patients who will undergo urologic manipulation. Patients undergoing urologic procedures should be treated with oral fluconazole OR AmB deoxycholate, before and after the procedure.
Treatment for Vulvovaginal Candidiasis
Topical antifungal agents, with no one agent superior to another, are recommended for the treatment of uncomplicated Candida vulvovaginitis. Alternatively, a single oral dose of fluconazole may be used.
Treatment for Oropharyngeal Candidiasis
Clotrimazole troches, 10 mg 5 times daily, or miconazole mucoadhesive buccal 50-mg tablet applied to the mucosal surface over the canine fossa once daily for 7–14 days is recommended for mild disease. Antiretroviral therapy is recommended to reduce the incidence of recurrent infections in HIV patients.
Treatment for Esophageal Candidiasis
A diagnostic trial of antifungal therapy should be performed before an endoscopic examination. Systemic antifungal therapy is always required.
Source: Clinical Practice Guideline for the Management of Candidiasis: 2016 Update by the Infectious Diseases Society of America
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries