COVID-19-related myocarditis & pericarditis: How to treat
M3 India Newsdesk May 12, 2021
SARS-CoV-2 (Severe Acute Respiratory Syndrome-CoV-2) presents an unprecedented threat to the global healthcare system. The virus has also been linked to myocarditis in patients, among other complications. This article throws light on the most likely pathophysiology of SARS-CoV-2–related myocarditis, pericarditis, and management of the conditions.
For our comprehensive coverage and latest updates on COVID-19 click here.
Infection by SARS-CoV-2
COVID-19's primary clinical manifestation is a respiratory infection, which can range from mild flu-like disease to serious pneumonia and ultimately fatal acute respiratory distress syndrome. The early mode of SARS-CoV-2 infection is viral attachment to the membrane-bound form of angiotensin-converting enzyme 2 (ACE2) by a protein called SPIKE (S protein) displayed in the viral coat, preceded by priming by the serine protease TMPRSS2, which mediates virus uptake. ACE2 is a membrane-bound peptidase found in all tissues but is particularly abundant in the lung, heart, vessels, kidney, brain, and GIT.
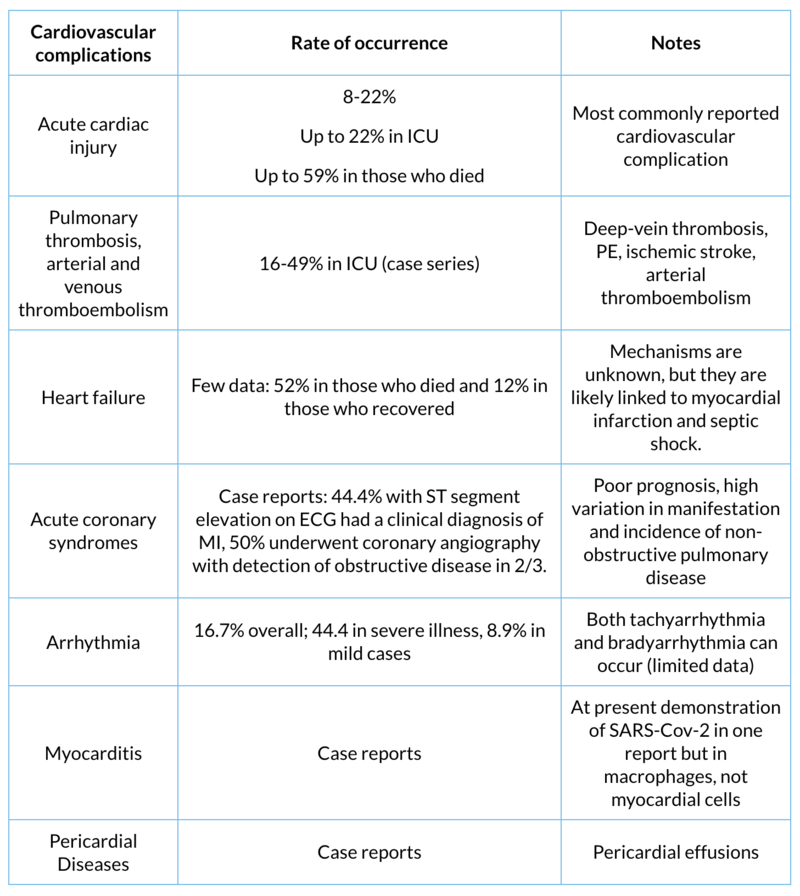
All of these organs are possible favoured targets for the virus on this basis, which may describe some findings of lung, heart, vessel, brain, and bowel complications, and also symptoms and signs associated with their involvement during COVID-19 infection. SARS-CoV-2 infection is possible in cardiovascular tissues or cells that express ACE2, also including lung cells. COVID-19 has been linked to myocarditis, pericardial effusion, and pericarditis among cardiovascular complications.
SARS-CoV-2 and myocarditis
SARS-CoV-2 may attack myocardial cells, and myocarditis has been identified in a small series from China, where 7% of deaths were due to myocardial injury with cardiovascular collapse without a direct, definitive diagnosis of myocarditis. Other studies have identified fulminant myocarditis with a high viral load and an inflammatory mononuclear infiltrate in myocardial tissue at autopsy, but no proof of explicit COVID-19 infection in the myocardium.
Troponin elevation alone cannot be used to diagnose myocarditis, and additional data is often unavailable. The majority of cases should be classified as scientifically suspected. Troponin elevation in the presence of COVID-19 can be attributed to a variety of factors like:
- Non-ischaemic myocardial injury (more likely) caused by various potential causes (e.g., intense hypoxia, sepsis, systemic inflammation, pulmonary thromboembolism, cytokine storm, stress cardiomyopathy) instead of a typical viral lymphocytic myocarditis
- Ischaemic myocardial injury caused by various possible mechanisms (e.g., severe hypoxia, sepsis, systemic inflammation, pulmonary thrombo (e.g., plaque rupture, coronary spasm, microthrombi, or direct endothelial or vascular injury). Concurrent renal dysfunction may worsen troponin elevation in both situations.
Pericardial diseases
Myocardial damage is common in COVID-19 patients who are hospitalised. Furthermore, higher troponin levels in COVID-19 patients are linked to a higher risk of mortality. There are two potential situations to mention in case of pericardial diseases like:
- A patient with pericarditis who can become infected with SARS-CoV-2 after being treated for it.
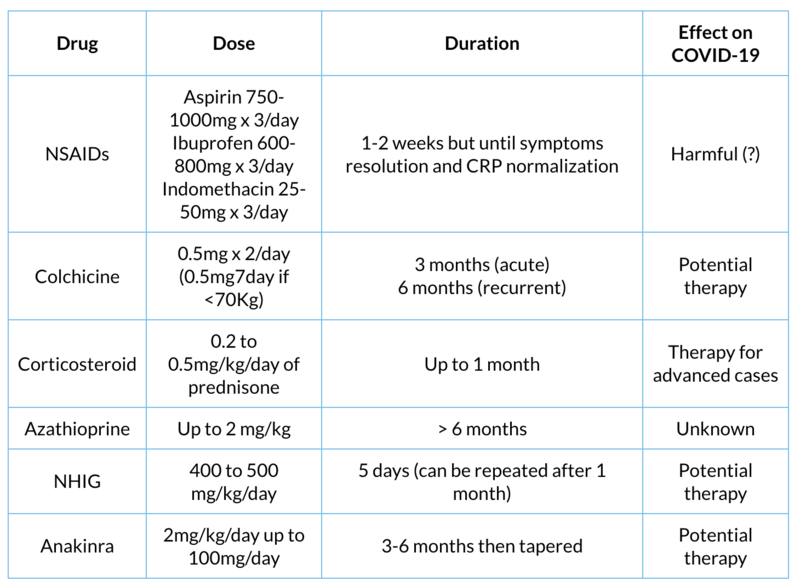
- A patient with COVID-19 who experiences pericarditis or pericardial effusion after being treated for it. Clinicians may be concerned about the safety of nonsteroidal anti-inflammatory medications (NSAIDs), corticosteroids, colchicine, and biological agents such as anti-IL1 agents (e.g., anakinra), which are the mainstay of treatment for refractory cases in both situations.
At the latest, only a few cases of COVID-19-associated pericarditis and pericardial effusion have been reported. Troponin elevation has been linked to myocardial involvement in the majority of cases recorded.
Medication
While there is a caution against using NSAIDs in the presence of COVID-19 infection, most pericarditis medications, such as corticosteroids, colchicine, and anakinra, do not tend to be contraindicated in the presence of COVID-19 infection. Even though, where corticosteroids and anakinra are used, close surveillance for superimposed bacterial infections is necessary. On this basis, pericarditis therapies cannot be stopped in patients that are now using them for disease prevention. Indeed, these agents are currently being evaluated for effectiveness in the context of COVID-19 infection and could soon become established therapeutic options.
To summarise, the heart and vessels are possible targets for COVID-19, but no evidence of overt infection and proliferation of SARS-CoV-2 in heart cells has yet been discovered. Additional pathologic research and autopsy series will be critical in elucidating SARS-ability CoV-2's to affect the myocardium/pericardium specifically and induce myocarditis and pericarditis.
Click here to see references
Disclaimer- The views and opinions expressed in this article are those of the author's and do not necessarily reflect the official policy or position of M3 India.
The author is a practising super specialist from New Delhi.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries