COVID-19: How will it likely end in India?: Dr. Purvish Parikh
M3 India Newsdesk Dec 24, 2020
After COVID-19 taking over our lives this year, we finally see a sliver of hope via a vaccine. But that aside, there could be other ways COVID-19 could wane or end in India. As we move into the new year, Dr. Purvish Parikh speculates various endgame theories for the pandemic will play out into the new year.
To read other originals by Dr. Purvish Parikh, click here.
For our comprehensive coverage and latest updates on COVID-19 click here.
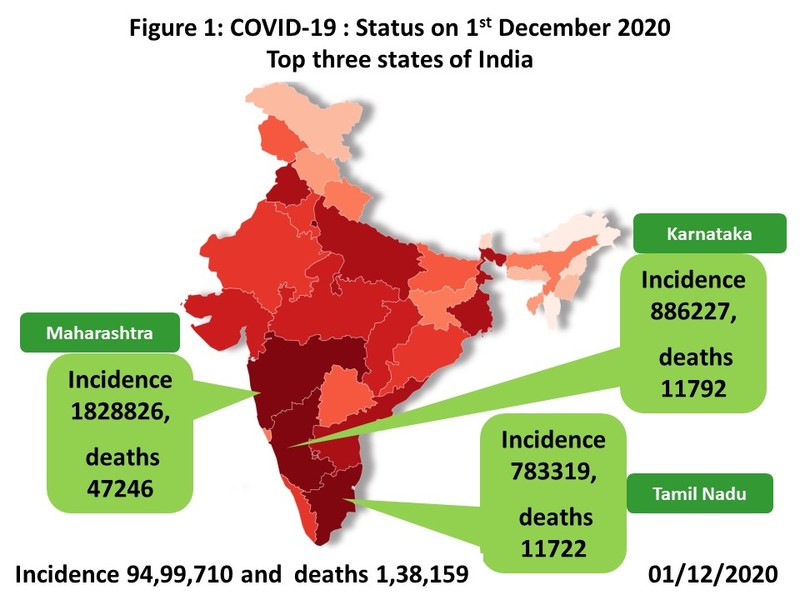
While the first COVID-19 case was officially reported from Wuhan in December 2019 (actually it was identified on 17th November 2019), India identified its first case on 30th January 2020. As of 1st December 2020, the states with the largest numbers are Maharashtra (incidence 1828826 , deaths 47246); Karnataka (incidence 886227, deaths 11792); and Tamil Nadu (incidence 783319, deaths 11722) (Figure 1).
India saw its peak in the week beginning 2nd September with daily new cases almost touching one lakh (97,859). By the end of November this had steadily and consistently reduced by two third (31,179 on 30th November). Similarly, the total number of active cases peaked (10,14,649) on 18th September and dropped to less than half (4,37,000) on 30th November. This was also mirrored by daily death rate of 1283 on 15th September (other than the spike of 2006 on 16th June due to reporting delays/bunched reporting by private hospitals) which dropped to 482 on 30th November.
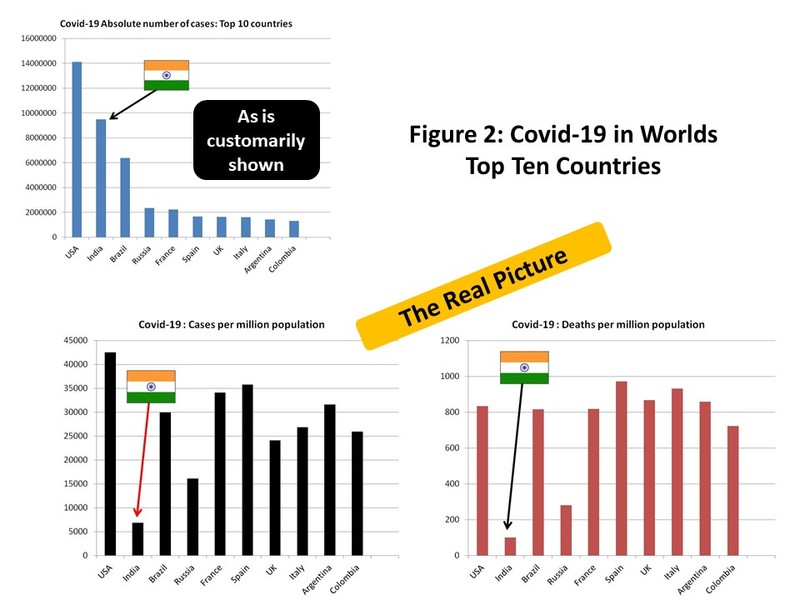
If we look at the top 10 countries in the world in terms of the largest number of COVID-19 cases (USA, India, Brazil, Russia, France, Spain, UK, Italy, Argentina and Colombia), the real picture is seen when we compare their rates per million of their population (Figure 2). While the remaining nine have rates in the five digits (15,909 to 42,519), in India we have only 6,856 cases per million of our people. Some have argued that this is because testing is inadequate in India. This is also not true. Our country has done a total of 141,349,298 COVID-19 tests, which translates to 102,007 tests per million of the population (10%). Whether this testing is enough or not is clear when we look at the number of tests required to pick up one positive case; it being 14.87 tests in India (which is more than the 13.9 tests in USA, 9.26 tests in France and 13.74 tests in Spain).
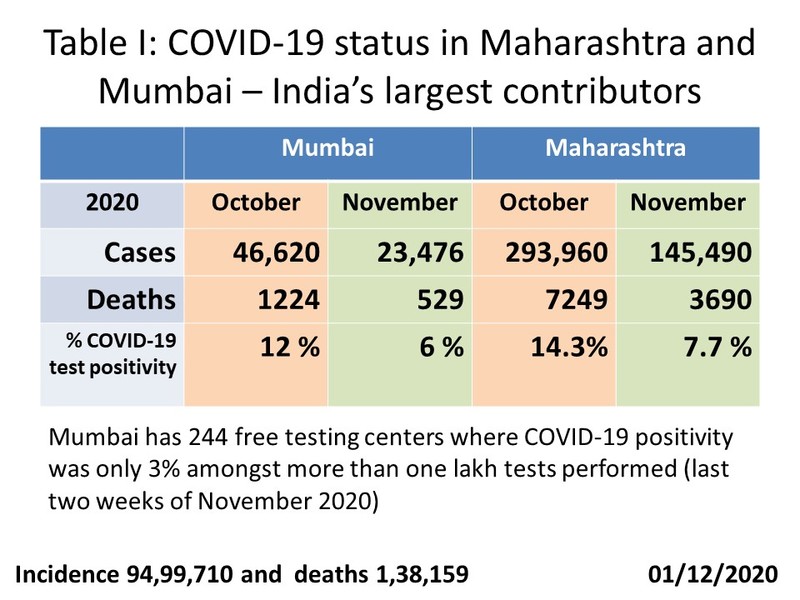
What has happened in the last two months is very interesting and give us hope that the end of the COVID-19 pandemic is nearer than thought just a few months ago (Table I). November saw consistent reduction in new cases, deaths and percentage of COVID-19 test positivity in both Mumbai and Maharashtra. In fact, Mumbai had added 244 free testing centers for the public, where COVID-19 positivity was only 3% amongst more than one lakh tests performed.
Endgame possibilities
The classical epidemiological end point of any pandemic occurs when herd immunity reaches sufficient level to prevent or attenuate transmission in the community. This could be a natural process by itself or hastened by vaccination. We could also consider an end point where the world returns to normalcy (when social, commercial and professional life becomes as normal as possible allowing the general public to return to earning their livelihood). This would be similar to the concept of functional cure - when COVID-19 is no longer expected to have long-term health related consequences. This would require a serious commitment and meticulous implementation of public health policies - a scenario that is not sustainable in most countries. For instance, two antibodies have recently received regulatory approval (Bamlanivimab of Eli Lilly by US FDA on November 9 whereas REGN-COV2 Regeneron received EUA license on November 22). However, these are expensive medicines that have limited application - post exposure injections to reduce hospitalisation in high-risk individuals.
As we begin to see the light brighten at the end of the tunnel, the question in the minds of most people is how is the COVID-19 pandemic likely to end?
Let us consider the following possibilities:
Death of homosapians
History teaches us about several highly infectious outbreaks that have decimated significant percentage of the global population. The archieological sites of Hamin Mangha and Miaozigou in China are our world's earliest known evidence (approximately 5000 years BCT) of mass deaths likely to be due to an epidemic. Antonine Smallpoox "Plague" is estimated to have killed over 5 million people in the Roman empire between AD 165 and 180. In AD 541-542, bubonic plague affected the Byzantine Empire in the midst of its glory. This is said to have killed 10% of the world's population. The Black Death (1346-1353) was caused by Yersinia pestis and wiped out more than 50% of Europe's population.
Jumping to 1918-1920, the so called Spanish Flu affected 500 million people and 100 million succumbed to it. Similarly the Asian Flu pandemic, starting from China killed 1 millon people (1957-1958). The AIDS pandemic that started in 1981 is still ongoing. It has already killed 35 million across the globe. However things have been different thereafter. The Swine Flu (2009-2010; caused by H1N1 virus) affected 1.4 billion people but killed less than 500,000. And the effects of the more recent Ebole and Zikaa epidemics have been limited.
Fear has also been fueled by several sci-fi movies that portray scenarios where only a few humans survive virulent infections - particularly due to unknown samples from outer space that devastate earths fragile bioecosystem. We believe that such a scenario is not likely to happen due to the current COVID-19 pandemic.
Cure
Advances in biotechnology, computational power, artificial intelligence and better understanding of lifesciences have led to personalized and precision medicine. Several hitherto fatal conditions are now either easily cured or their natural history converted into a chronic ailment that is easily controlled. This has been as a result of new inventions of drugs that specifically target the disease like imatinib for chronic myeloid leukaemia, trastuzumab for Her2 positive breast cancer, infiximab for ulcerative colotis/rheumatoid arthritis and Car T cell therapy.
Drugs that have been studied for COVID-19 include high dose corticosteroids, hydroxychloroquine, azithromycin, ramdesivir, tocilizumab, ivermectin, convalescent plasma therapy (CPT), and low molecular weight heparin. None of these (or any other) drugs have yet been proven to be effective for the treatment of COVID-19 and hence are only used off label on compassionate basis for select individuals. With more than 64 million people affected worldwide and almost 1.5 million dead in the span of less than one year, all attempts by the pharmceutical industry to come up with effective treatment have been unsuccessful. So we believe that pharmacological cure for COVID-19 is very unlikely.
The virus fades away
There is a theoretical possibility that the virus will simply vanish, just as it "spontaneously" appeared. COVID-19 has been proven to have undergone several mutations in various parts of the world. If this continues, mutations might make the virus unstable, unable to tolerate the environment, lose it virulence or simply self-destruct.
The last time this happened was after the Black Death of 1346-53, when the strain of Yersinia pestis that killed half of Europe disappeared. But it did not happen with HIV, Ebola or Zika. And the coronavirus group of family seem to raise their ugly head far too frequently of late.
Immunity
While the COVID-19 pandemic is in its second global peak, there are some parts of the world where the mortality rate is much lower than expected. There have been several postulations regarding existence of innate immunity against this virus. We have previously published that it could be due to BCG vaccination, exposure to malaria parasite (which carries viral particles similar to COVID-19) or simply racial genomic differences. In the same family, people respond differently to exposure to the virus. One spouse lands up in ICU whereas the other one remains essentially asymptomatic.
Curiously, a pregnant lady in Singapore was found to be infected with COVID-19 in the first trimester. She had mild symptoms, was briefly hospitalised and remained well for the remaining part of her pregnancy. She recently delivered a healthy baby who was found to have antibodies against COVID-19. Couple this with the fact that, so far, COVID-19 has never been documented either in the amniotic fluid or in breast milk. Clearly this is good news for pregnant mothers as well as newborns. China has also reported that such protective antibodies titers exist in newborns but tend to fall with time.
The fall in protective IgG antibody titres has been well documented amongst patients infected with COVID-19, irrespective of severity of the illness. Does this mean that the acquired immunity is temporary? We do not know the answer. There have been several instances of clearly documented second infections amongst people in Hong Kong, China, India and other countries. Repeat exposure to the virus can rekindle body's immunity - via the T lymphocytes and memory cells. Immune response could also be related to IgA antibodies located within the mucosal membranes, the point of entry of the virus into human bodies.
Herd immunity has been hotly debated with vehement arguments supporting both sides. The recently published data in The Lancet from a large prospective study on convalescent plasma therapy conducted by Dr. Sandeep Budhiraja and others have clearly shown that patients with serious COVID-19 illness benefit. This is good indirect evidence of the value of "herd" immunity - at least amongst previously infected persons. Couple this with the reports of high antibody levels in people who have had mild or no symptoms and never required hospitalisation.
Does this mean that minor exposure to the virus can lead to development of immunity without suffering from the illness? Community antibody testing have also supported this concept. While protective antibodies against COVID-19 in the community were 14% in Stockholm, and 21% in New York, Mumbai reported world's highest level - a massive 57% amongst 6936 people tested from Dharavi (as reported by the municipal corporation in a study conducted in collaboration with Tata Institute of Fundamental Research in May 2020; Dharavi is Asia's biggest slum consisting of about 10,00,000 low income people residing in crowded high density accommodation).
Another study reported on 28th November, provides further insight. This was done between October 5 to October 10 in slum areas of Colaba, south mumbai. A total of 806 people were tested of which a whopping 605 (75%) were found to be antibody positive. Interestingly, only 1% of them had been previously diagnosed to have suffered from COVID-19, indicating that most of the people with immunity had no or mild symptoms of their infection. Clearly, India is ahead of the global curve in terms of herd immunity against COVID-19; and can be a plausible reason for the end of the pandemic here.
Vaccine
In the race for vaccines against COVID-19, Pfizer is the winner having received emergency regulatory approval from the UK on 2nd December 2020. At least four to six other candidates are not far behind. With preliminary reports indicating success rates of about 90% coupled with a good safety profile, are these indications of a brighter pandemic free future just round the corner?
The question has now shifted, from if to when. This is the most promising path leading to success over the current COVID-19 pandemic.
We can look forward to this endgame scenario by 2021 - India likely to be ahead of the western world by three to six months.
A word of caution- setback in these optimistic projections could happen due to a number of real world issues - remember Murphy's laws? We need to pay close attention to vaccine safety, manufacturing, supply chain, government policy (especially prioritising right, vulnerable populations), rollout implementation, community acceptance and long term vaccine efficacy (especially immunity after the protective antibody levels taper off). Having said that, as Christmas approaches, we can end 2020 with something to cheer about.
Disclaimer- The views and opinions expressed in this article are those of the author's and do not necessarily reflect the official policy or position of M3 India.
The author, Dr. Purvish Parikh is a Precision & Medical Oncologist from Mumbai.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries