Clinical Outcomes of Hemodiafiltration in Dialysis
M3 India Newsdesk Sep 25, 2023
Patients with Chronic Kidney Disease (CKD) on dialysis are a severely ill population with a complex comorbidity situation and high mortality rates. Haemodiafiltration (HDF) offers the potential to improve hard clinical outcomes, and clinical studies have shown very promising results.
Haemodiafiltration (HDF) overview
There is a clear need to improve the hard clinical endpoints and the quality of life of ESRD patients. Most of the patients depend on extracorporeal renal replacement therapy, such as low- and high-flux haemodialysis (HD) or haemodiafiltration (HDF). HDF is in widespread use, especially in Europe, but less so in the United States and Asia with very few centres in India.
HDF combines the diffusion of mainly low molecular weight uremic toxins, known from conventional HD, with the convection of soluble middle-sized toxins, such as β2-microglobulin, within the same high-flux haemodialyser module.
HDF is considered the most advanced renal replacement therapy that is currently available, as clinical studies have demonstrated its superiority in removing middle- and large-sized uremic toxins as compared to HD.
Technical considerations
It is a form of kidney replacement therapy that combines the principles of HD and haemofiltration (HF). In conventional HD, solute removal is primarily achieved via diffusion, which is the movement of molecules along a concentration gradient between the blood and dialysate that is higher for small molecules. In contrast, solute removal in HF is based on convective transport, which depends on the ultrafiltration rate and is equal for different molecule sizes as long as they can pass through the pores of the membrane, reflecting its sieving capacity.
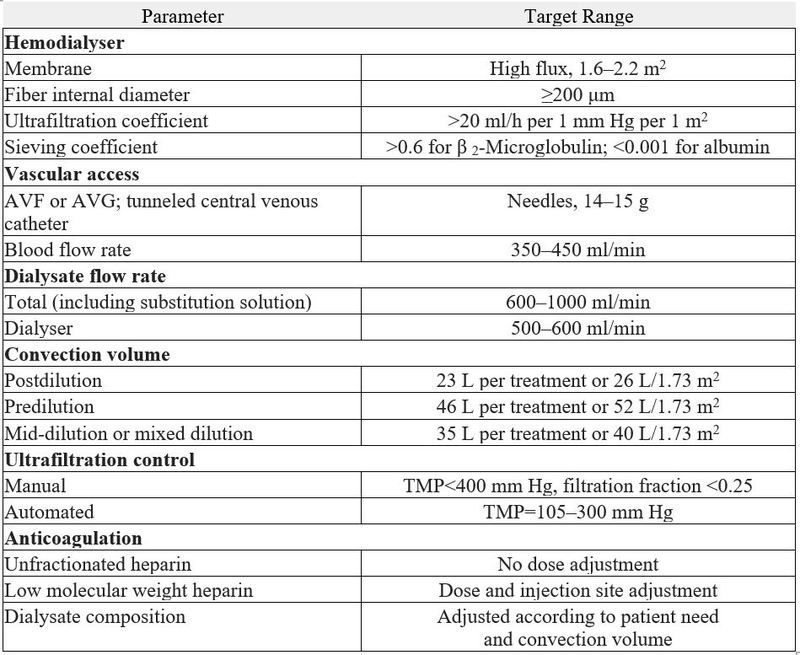
The following components are required to perform HDF:
1. HDF machine
These machines are capable of online preparation of substitution fluid by adding three components to conventional HD machines;
- A pump for delivering substitution fluid.
- A series of specifically qualified sterilising ultrafilters to produce sterile substitution fluid from the dialysate.
- A system for controlling fluid exchange to achieve the desired convection volume and net fluid removal.
2. Haemodiafilter
There are three requirements of a haemodiafilter that differentiate it from a standard HD dialyser, which is as follows:
- A sharp sieving coefficient curve to maximise the convective solute removal while retaining albumin.
- High permeability to maximise the ultrafiltration volumes during HDF treatments.
- A fibre geometry optimised to mitigate the effects of haemoconcentration.
3. Substitution fluid
HDF removes high plasma water volumes via ultrafiltration, which, in turn, needs to be replaced iso-volumetrically with a substitution fluid. This substitute fluid is infused into the blood of the patient and, therefore, needs to be sterile and non-pyrogenic. HDF machines include an infusion pump that can infuse substitution fluid into the blood at different points in the extracorporeal circuit, including the venous line (post-dilution), the arterial line (predilution), and the blood compartment of the dialyser (mid-dilution).
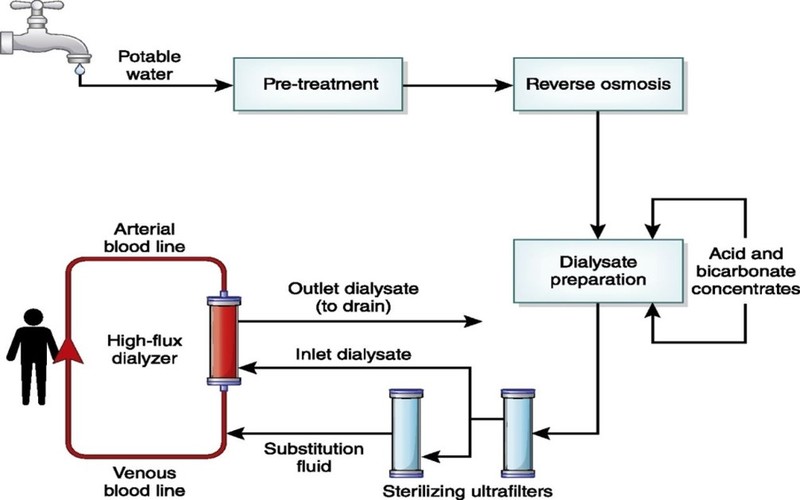
HDF circuit
Prescription of HDF
Treatment schedule 3 sessions of 4 hours weekly (minimum), longer or more frequent (possible).
Advantages of HDF
- Haemodynamic stability with increased tolerance of fluid loss
- Blood pressure control
- Reduction in the incidence of muscle cramps, arrhythmia, headache, pruritus, vomiting and post-dialysis fatigue
- Reduction in all-cause mortality
- Decreases oxidative stress and inflammation and improves endothelial function
- Improves Anaemia control by increasing EPO sensitivity
- Decreases B2-M-related amyloidosis
- Improves phosphate control
Limitations of HDF
- High price cost
- Infrastructure and availability
- Patient factors like poor blood flow from vascular access
- Increased risk of infection
Current scenario and future directions
In India, there are very limited centres which are doing HDF due to its limitations, especially the price related to it. Evidence regarding the superiority of HDF vs. HD with regard to patient-related outcomes is still scarce, and even in terms of mortality, the debate is still ongoing.
In conclusion, there is more and more evidence that HDF delivered at a high dosage improves performance as compared to standard HD treatments. Furthermore, HDF is associated with better clinical outcomes for traditional or hard endpoints, such as all-cause and cardiovascular mortality.
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr Bhavin Mandowara is a practising nephrologist at Zydus Hospital, Ahmedabad.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries