Chronic Constipation in Adults: Guideline by Indian Society of Gastroenterology
M3 India Newsdesk May 16, 2023
In Indian cultures and clinical practice, chronic constipation (CC) is a prevalent issue. This article presents the 29 key statements made by the Indian Motility and Functional Diseases Association and the Indian Society of Gastroenterology on chronic constipation.
A recent article that predated this consensus publication reviewed the long-held belief of Indian experts that the epidemiology, clinical spectrum, diagnostic assessment, treatment needs, and patient expectations among patients with CC in India were somewhat different from the West.
As a result, it was thought crucial to evaluate the published Indian data, and in the lack of suitable literature, a choice based on the experience of Indian professionals as a whole had to be made to direct doctors treating these patients. The current CC consensus was thus started.
This evidence-based practice guideline for managing chronic constipation was created by the Indian Motility and Functional Diseases Association and the Indian Society of Gastroenterology and published in the Indian Journal of Gastroenterology in Jan 2019.
Statements of consensus
Statement No. 1: Chronic constipation is widespread in India.
Despite the dearth of information, the studies that are currently available show that CC is a widespread health issue in India, debunking the myth that it is uncommon there because of vegetarianism, high-fibre diets, and more frequent bowel movements. This suggests that CC may be underreported.
Statement No. 2: In India, stools occur more often and with softer consistency.
Bristol stool forms connect inversely with colon transit time; shorter transit time is related to higher scores. As a result, the stools of Indian patients are softer than those of individuals from the West.
Statement No. 3: Instead of focusing on stool frequency, India should define constipation based on the types of faeces and how patients perceive it.
The Western definition of CC, which calls for a stool frequency of fewer than three times per week, is predicted to be insensitive in the Indian population due to the greater daily bowel frequency.
Statement No. 4: Bristol types I–III, which are described as stools associated with constipation, are more sensitive to CC diagnosis in India than Bristol types I–II are in the West.
The definition of CC by Bristol kinds I–II stool forms, as suggested in the West, may ignore a significant part of patients since Indians pass softer stools.
Statement No. 5: Functional constipation is more prevalent than IBS-C in India because gastrointestinal discomfort is less severe and less frequent.
Statement No. 6: Patients with CC often have abdominal bloating.
As many as 80% of IBS sufferers may describe experiencing stomach bloating. However, even though the Asian diagnostic criteria did include it, it is not listed as one of the crucial symptoms in the Rome IV diagnostic criteria. Compared to individuals with IBS-D, patients with IBS-C have increased abdominal bloating and/or distention.
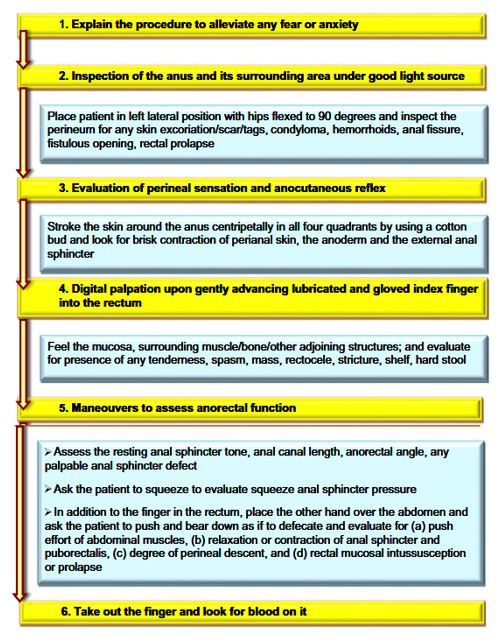
Statement No. 7: Identification of faecal evacuation disorder requires a thorough clinical assessment that includes a digital rectal exam and the patient's medical history.
A thorough clinical assessment, which includes a digital rectal examination (DRE), may often be used to suspect and diagnose Faecal Evacuation Disorder (FED).
Statement No. 8: Fever and delayed transit constipation is not disregarded if the IBS criteria are met.
FED and slow transit constipation (STC) cannot be ruled out by these symptoms alone, despite the Rome Foundation and Asian consensus having precisely established criteria for the diagnosis of IBS.
Statement No. 9: Women are more likely than males to have Faecal Evacuation Disorder.
Most Western investigations on FED revealed a female predominance, and it is often held that men are less likely to develop FED. However, a few hospital-based Indian surveys showed that FED also affects the male population. Given that one of the risk factors for FED is pelvic floor damage during delivery, it is anticipated that the frequency of FED would be greater in women.
Statement No. 10: Lifestyle variables, a few systemic diseases, several medications, and physiological anomalies like FED and slow colon transit all have a role in CC.
In epidemiological studies, lifestyle variables such as inadequate dietary fibre and fluid intake, irregular and insufficient bathroom use, sedentary behaviour, extended bed rest, systemic diseases, and chronic drug use that causes CC have all been identified as risk factors.
Statement No. 11: Pelvic floor and anorectal disorders may be brought on by obstetric stress.
The pelvic floor muscles must be functionally integrated for defecation and continence. During childbirth, pelvic connective tissue, nerves, and muscles can suffer damage that leads to pelvic floor dysfunction (PFD).
PFD in this situation may present as incontinence, rectocele, haemorrhoids, rectal prolapse, or severe constipation. Older age, increased parity, and vaginal birth are risk factors for PFD in females.
Statement No. 12: An Indian toilet is more physiological for defecation than a Western toilet.
Culture-specific defecatory postures include squatting and sitting, which are the most prevalent positions globally. Traditional Japanese and Indian toilets call for squatting, although more people are rapidly transitioning to Western-style toilets in India's cities. A recent study from Japan comparing three defecation postures—squatting, sitting, and sitting with the hips flexed at 60° by placing the feet on a height-adjustable step—found that squatting had the lowest basal abdominal pressure before defecation and the widest recto-anal angle when compared to both sitting postures.
Statement No. 13: Bristol stool shape and colon transit are correlated.
In patients who are constipated, stool form is often utilised as a clinical substitute for colon transit. For more than 20 years, the Bristol stool form scale (BSFS) has been used in clinical settings.
Statement No. 14: A subgroup of individuals with CC have been demonstrated to have certain pathophysiological abnormalities at the molecular level (myopathic, neuropathic, and others).
Statement No. 15: Gut transit is slowed by excessive methane production, which is linked to CC.
Healthy individuals have methane-producing bacteria in their guts in between 30% and 62% of cases. Methane reduces GI motility, according to research conducted in vitro and in vivo, hence its quantity may be negatively related to the type and frequency of stools.
Statement No. 16: Patients with CC often have psychological problems.
IBS and CC are two examples of functional gastrointestinal diseases (FGIDs) that have been linked to psychological illnesses. Numerous CC patients have signs of a current or past psychotic disorder.
Statement No. 17: FED is related to solitary rectal ulcer syndrome.
All age groups are affected by the chronic benign condition known as solitary rectal ulcer syndrome (SRUS), which manifests as rectal bleeding, leucorrhea, tenesmus, constipation, and a sense of incomplete evacuation.
Statement No. 18: Age more than 45 years old, a visible or occult GI bleed, a family history of colon cancer, unexpected weight loss, an abdominal mass, and fever are alarm features that may call for invasive investigations like a colonoscopy.
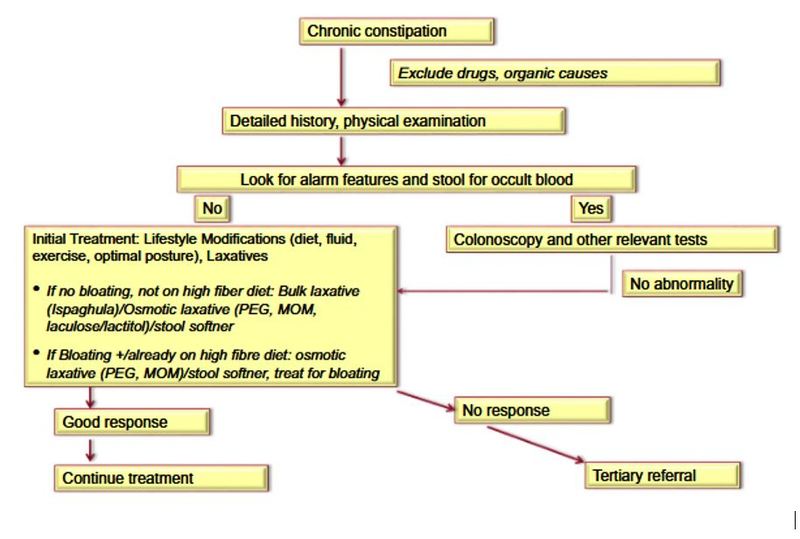
Statement No. 19: Osmotic laxatives and lifestyle changes should be part of the first therapy for CC.
Even though they are not the only causes, a variety of lifestyle factors may contribute to CC in some patients. Furthermore, despite the limited scientific evidence supporting their efficacy, doctors may advise patients to follow these simple, safe, healthy, and easy practices. These precautions include getting enough dietary fibre, drinking lots of water, exercising often, and maintaining normal sleep patterns. In people with CC, the position used when urinating may have consequences.
Statement No. 20: If the patient is currently eating a high-fibre diet and/or stomach bloating is a noticeable symptom, a fibre supplement should be avoided.
Many medical professionals advise using fibres as the first line of treatment for CC, especially if dietary fibre intake is low and bloating is not a prominent symptom.
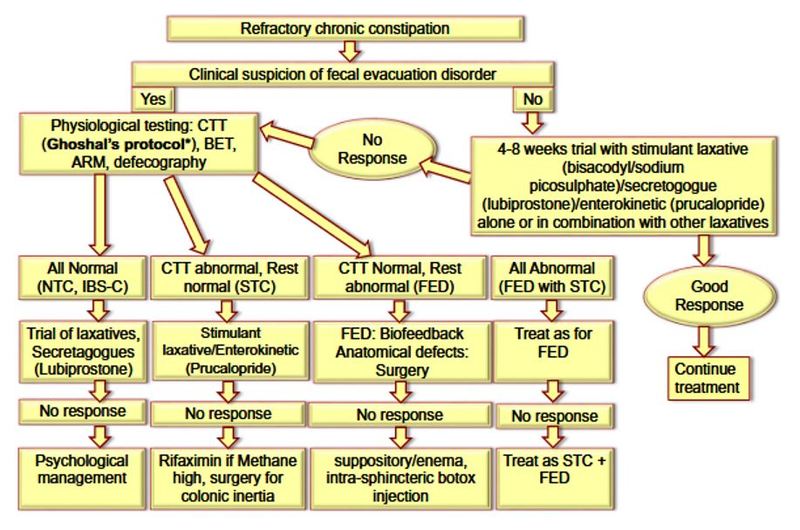
Statement No. 21: Pathophysiological issues including sluggish intestinal transit and FED should be looked at in patients who are resistant to the first therapy.
A refractory disease at tertiary institutions has to be explored for complex pathophysiological concerns, which are not uncommon, even if the majority of patients coming to primary care centres may have minor constipation and lifestyle and nutritional variables contributing to their symptoms.
Statement No. 22: To check for FED, a thorough rectal examination that measures the pressure and relaxation during rest and attempted section is helpful.
Statement No. 23: The colonic transit research procedure used in the West may not work as effectively in India.
The colon transit time (CTT) evaluation procedure devised in Western nations may not stand up well in India because the transit is substantially quicker
Statement No. 24: For the diagnosis of FED, several test positives, such as the balloon expulsion test, anorectal manometry, and defecography, are more accurate than just one test.
Statement No. 25: In the open healthcare system of India, especially in the tertiary care setting, the top-down strategy may be favoured in certain patients with CC.
The basic goal of CC treatment is to reduce symptoms. The majority of patients that enter tertiary-level healthcare settings have previously undergone the majority of traditional therapy, including dietary and lifestyle changes as well as typical laxatives.
Therefore, it is unlikely that most of these patients will improve and be satisfied with the step-up approach suggested by the most recent recommendations. Instead of going top-down, a more feasible alternative could be to go up from the level at which the patient has previously been treated.
Statement No. 26: Medicines encouraging colonic motility should be favoured for the management of slow transit constipation.
Colokinetic medications should be used to treat STC since they focus on the main pathophysiological problem. The 5HT4 agonist prucalopride increases intestinal motility.
Statement No. 27: For FED, biofeedback needs to be used as the first therapy.
In Indian research, symptoms significantly improved in 14 (70%) of 20 patients who completed more than four biofeedback sessions.
Statement No. 28: Surgery should only be performed on individuals with refractory CC who have certain structural or functional problems.
Statement No. 29: Before receiving surgical treatment, a psychological examination is required.
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr Monish Raut is a practising super specialist from New Delhi.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries