Cardiovascular Complications of Diabetes Mellitus
M3 India Newsdesk Apr 16, 2024
Delve into the intricate connection between diabetes and cardiovascular disease, uncovering the hidden risks and multifaceted strategies for prevention and management. Explore how intertwined metabolic pathways and targeted therapies shape the landscape of diabetic cardiovascular complications.
Beyond diabetes's immediate effects on glucose metabolism, diabetes significantly increases the risk of developing cardiovascular complications. These complications pose a grave threat to individuals with diabetes, often leading to significant morbidity and mortality. Understanding the intricate relationship between diabetes and cardiovascular disease is crucial for effective prevention, management, and treatment strategies.
Pre-diabetes, defined as impaired glucose tolerance, impaired fasting glucose, or raised HbA1c, was associated with an increased risk of cardiovascular disease. The health risk might be increased in people with a fasting glucose concentration as low as 5.6 mmol/L or HbA1c of 39 mmol/mol.
The interplay between diabetes and cardiovascular disease
Diabetes and cardiovascular disease share a complex interplay of pathophysiological mechanisms. Individuals with diabetes often exhibit a cluster of risk factors collectively termed "diabetic dyslipidemia," characterised by elevated levels of triglycerides, decreased levels of high-density lipoprotein (HDL) cholesterol, and increased levels of small, dense low-density lipoprotein (LDL) particles. These lipid abnormalities contribute to the development of atherosclerosis, a key process underlying cardiovascular disease.
Recent studies have found that rates of incident heart failure hospitalisation were two-fold higher in people with DM when compared with the population without DM. The patient may present with a wide spectrum of heart failure.
Moreover, chronic hyperglycemia in diabetes leads to the formation of advanced glycation end-products (AGEs), oxidative stress, and activation of inflammatory pathways, all of which promote endothelial dysfunction and vascular inflammation. These processes further accelerate atherosclerosis and increase the risk of cardiovascular events such as myocardial infarction, stroke, and peripheral artery disease.
Specific cardiovascular complications associated with diabetes
- Coronary Artery Disease (CAD): Individuals with diabetes are at a substantially higher risk of developing CAD compared to those without diabetes. The presence of diabetes confers a two to fourfold increase in the risk of coronary events. Furthermore, diabetes is often associated with atypical symptoms of myocardial ischemia, leading to delayed diagnosis and management of CAD.
- Stroke: Diabetes significantly increases the risk of ischemic stroke, primarily through its effects on atherosclerosis and small vessel disease. Moreover, individuals with diabetes who experience a stroke have a poorer prognosis and a higher likelihood of disability and mortality compared to non-diabetic stroke patients.
- Peripheral Artery Disease (PAD): Diabetes is a major risk factor for PAD, a condition characterised by narrowing or blockage of the arteries supplying the legs and feet. PAD in diabetes often presents as intermittent claudication, ulcers, or non-healing wounds, and is associated with an increased risk of lower extremity amputation.
- Heart failure: Diabetes is an independent risk factor for the development of heart failure, both with reduced and preserved ejection fraction. The mechanisms underlying diabetic cardiomyopathy involve metabolic abnormalities, oxidative stress, inflammation, and myocardial fibrosis, leading to impaired cardiac function over time.
Prevention and management strategies
Given the profound impact of diabetes on cardiovascular health, effective prevention and management strategies are paramount. Lifestyle modifications, including healthy eating habits, regular physical activity, smoking cessation, and weight management, play a central role in reducing the risk of cardiovascular complications in individuals with diabetes.
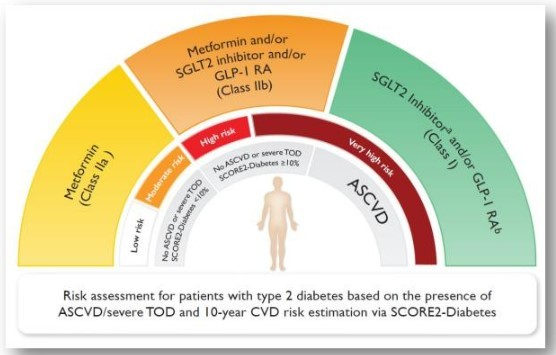
Furthermore, aggressive management of cardiovascular risk factors such as hypertension, dyslipidemia, and hyperglycemia is essential. Pharmacological interventions, including statins, angiotensin-converting enzyme (ACE) inhibitors, angiotensin receptor blockers (ARBs), and antiplatelet agents, are commonly used to reduce cardiovascular risk in diabetic patients.
Cardiovascular disease and T2D
Managing cardiovascular disease (CVD) in individuals with diabetes requires a multifaceted approach that often involves the use of various medications.
Here are some commonly used drugs in the management of CVD in diabetes:
- Statins: They are recommended as first-line therapy for individuals with diabetes and CVD or at high risk of CVD due to their proven efficacy in reducing cardiovascular events. With maintenance of LDL levels below 55mg/dl in high-risk patients. If desired levels are not achieved with a statin alone addition of ezetimibe followed by bempedoic acid should be considered.
- ACE Inhibitors (Angiotensin-Converting Enzyme Inhibitors) and ARBs (Angiotensin Receptor Blockers): These classes of medications are commonly used to treat hypertension and reduce the risk of cardiovascular events in individuals with diabetes.
- Beta-blockers: They are commonly prescribed to individuals with diabetes and CVD to manage hypertension, angina, and heart failure and to reduce the risk of recurrent myocardial infarction.
- Antiplatelet agents: Aspirin and other antiplatelet agents such as clopidogrel are commonly used in individuals with diabetes and CVD to prevent blood clots and reduce the risk of cardiovascular events, particularly in those with a history of myocardial infarction or stroke.
- Sodium-Glucose Co-transporter 2 (SGLT2) Inhibitors: In addition to their glucose-lowering effects, SGLT2 inhibitors have been shown to reduce the risk of heart failure hospitalisation and cardiovascular death in individuals with established CVD or at high cardiovascular risk.
- Glucagon-like peptide-1 (GLP-1) Receptor Agonists: They not only improve glycemic control but also have cardiovascular benefits, including a reduction in the risk of major adverse cardiovascular events in individuals with established CVD or at high cardiovascular risk.
- Diuretics: They are commonly used in individuals with diabetes and heart failure or hypertension to manage fluid retention and edema.
- Insulin: For individuals with diabetes and CVD, optimal glycemic control is essential to reduce the risk of cardiovascular complications. Insulin therapy may be required in those with inadequate glycemic control despite oral medications or in those with advanced diabetes complications.
- If the patient is already on dual therapy or multiple glucose-lowering therapies and not on an SGLT2 inhibitor or a GLP-1 receptor agonist, consider switching to one of these agents with proven cardiovascular benefits.
- Introduce SGLT2 inhibitors or GLP-1 receptor agonists in people with CVD at A1C goal (independent of metformin) for cardiovascular benefit, independent of baseline A1C or individualised A1C goal.
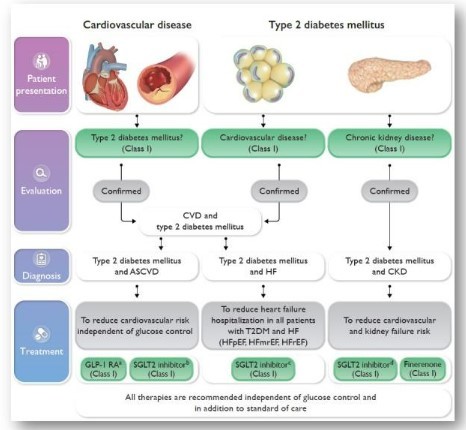
It's important to note that the choice of medications and treatment strategies should be individualised based on each patient's specific needs, comorbidities, and cardiovascular risk profile. Regular monitoring and close collaboration between healthcare providers, including cardiologists, endocrinologists, and primary care physicians, are essential to optimise cardiovascular outcomes in individuals with diabetes.
Conclusion
The cardiovascular complications of diabetes represent a significant clinical challenge, contributing to substantial morbidity and mortality worldwide. A comprehensive understanding of the pathophysiological mechanisms underlying these complications is essential for the development of targeted prevention and management strategies. By addressing modifiable risk factors and implementing evidence-based interventions, healthcare providers can mitigate the burden of cardiovascular disease in individuals with diabetes, ultimately improving patient outcomes and quality of life.
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr. Hitesh Saraogi is a diabetologist, physician and obesity specialist at Dhanvantari Hospital, Raj Nagar Extension, Ghaziabad.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries