Hyponatraemia: Causes and Treatment Approach
M3 India Newsdesk Jul 19, 2023
Hyponatraemia is the most common electrolyte disorder, with a prevalence of 20% to 35% among hospitalised patients. The pathogenesis and treatment of hyponatraemia are discussed in this article. The term SIADH (Syndrome of inappropriate antidiuretic hormone secretion) is also explained in the article.
Hyponatraemia
Hyponatremia is defined as a serum sodium concentration of less than 135 mEq/L but can vary to a small extent in different laboratories. Hyponatraemia is a common electrolyte abnormality caused by an excess of total body water when compared to total body sodium content.
The incidence of hyponatraemia is high among critical patients in the intensive care unit (ICU) and also in postoperative patients. This is more common in elderly patients due to multiple co-morbidities, multiple medications, and a lack of access to food and drinks.
Aetiology
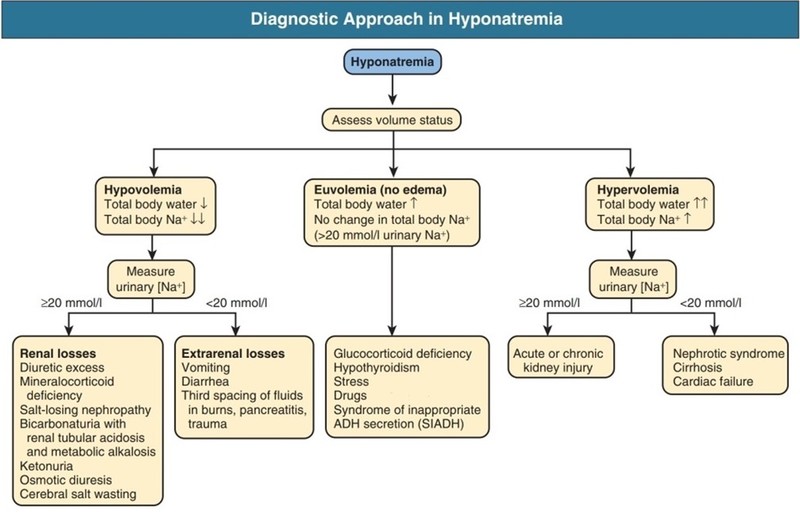
The aetiology of hyponatraemia can be classified based on the volume status of the extracellular fluid. Total body water (TBW) has two main compartments, extracellular fluid (ECF) accounting for one-third and intracellular fluid (ICF), accounting for the remaining two-thirds. Sodium is the major solute of ECF and potassium for ICF.
Based on the volume of ECF, a patient can be classified into hypovolemic, euvolemic, or hypervolemic.
Causes of Hypovolemic Hyponatraemia (TBW decreases more than a decrease in total body sodium)
- Gastrointestinal fluid loss (diarrhoea or vomiting)
- The third spacing of fluids (pancreatitis, hypoalbuminemia, small bowel obstruction)
- Diuretics
- Osmotic diuresis (glucose, mannitol)
- Salt-wasting nephropathies
- Cerebral salt-wasting syndrome
- Mineralocorticoid deficiency
Causes of Hypervolemic Hyponatraemia (TBW increases greater than an increase in total body sodium)
- Renal causes (acute renal failure, chronic renal failure, nephrotic syndrome)
- Extrarenal causes (congestive heart failure, cirrhosis)
- Iatrogenic
Causes of Euvolemic Hyponatraemia (TBW increase with stable total body sodium)
Nonosmotic, pathologic vasopressin release may occur in normal volume status, as with euvolemic hyponatraemia.
Causes of euvolemic hyponatraemia include:
- Drugs ( mentioned below)
- Syndrome of inappropriate antidiuretic hormone (SIADH)
- Addison's disease
- Hypothyroidism
- High fluid intake in conditions like primary polydipsia; or potomania, caused by a low intake of solutes with relatively high fluid intake
- Medical testing related to excessive fluids such as a colonoscopy or cardiac catheterisation
- Iatrogenic
Many drugs cause hyponatraemia and the most common include:
- Vasopressin analogues such as desmopressin and oxytocin.
- Medications that stimulate vasopressin release or potentiate the effects of vasopressin such as selective serotonin-reuptake inhibitors and other antidepressants morphine and other opioids.
- Medications that impair urinary dilution such as thiazide diuretics.
- Medications that cause hyponatraemia such as carbamazepine or its analogues, vincristine, nicotine, antipsychotics, chlorpropamide, cyclophosphamide, and nonsteroidal anti-inflammatory drugs.
Pathophysiology
Thirst stimulation, antidiuretic hormone (ADH) secretion, and handling of filtered sodium by kidneys maintain serum sodium and osmolality. Normal plasma osmolality is around 275 mOsm/kg to 290 mOsm/kg. To maintain normal osmolality, water intake should be equal to water excretion. The imbalance of water intake and excretion causes hyponatraemia or hypernatraemia.
SIADH (Syndrome of inappropriate antidiuretic hormone secretion)
This is a condition where inappropriate secretion of ADH despite normal or increased plasma volume causes impaired water excretion by the kidney leading to hyponatraemia. SIADH is a diagnosis of exclusion, as there is no single test to confirm the diagnosis. Patients are hyponatremic and euvolemic.
Causes of SIADH include:
- Any central nervous system (CNS) disorder
- Ectopic production of ADH (most commonly small cell carcinoma of the lung)
- Drugs (carbamazepine, oxcarbazepine, chlorpropamide, and multiple other drugs)
- HIV
- Pulmonary diseases (pneumonia, tuberculosis)
- Postoperative patients (pain medicated)
Approach to the patient
History and physical examination
Symptoms depend upon the degree and chronicity of hyponatraemia. Patients with mild-to-moderate hyponatraemia (greater than 120 mEq/L) or a gradual decrease in sodium (greater than 48 hours) have minimal symptoms. Patients with severe hyponatraemia (less than 120 mEq/L) or rapid decrease in sodium levels have multiple varied symptoms.
Symptoms can range from anorexia, nausea and vomiting, fatigue, headache, and muscle cramps to altered mental status, agitation, seizures, and even coma.
Apart from symptoms, a detailed history taking to include a history of pulmonary and CNS disorders, all home medications, and social history (increased beer intake or use of MDM or ecstasy) is very important.
Physical examination includes assessing volume status and neurological status.
Patients with neurological symptoms and signs need to be treated promptly to prevent permanent neurological damage
Steps for evaluation
The following steps may be performed while evaluating a patient with suspected hyponatraemia;
Step 1: Plasma Osmolality (275 mOsm to 290 mOsm/kg)
- It can help differentiate between hypertonic, isotonic, and hypotonic hyponatraemia
- True hyponatremic patients are hypotonic
- If the patient is hypotonic, then go to step 2
Step 2: Urine Osmolality
- Urine osmolality less than 100 mOsm/kg indicates primary polydipsia or reset osmostat.
- Urine osmolality greater than 100 mOsm/kg usually indicates a high ADH state, go to step 3
Step 3: Volume Status (ECF status)
- Hypovolemic vs. euvolemic vs. hypervolemic
- If the patient is hypovolemic, then proceed to step 4
Step 4: Urine Sodium Concentration
- Urine sodium less than 10 mmol/L indicates extrarenal loss of fluid (remote diuretic use and remote vomiting)
- Urine sodium greater than 20 mmol/L suggests renal loss of urine (diuretics, vomiting, cortisol deficiency, and salt-wasting nephropathies)
Other tests that might help in differentiating the causes include:
- Serum thyroid-stimulating hormone (TSH)
- Serum adrenocorticotropic hormone (ACTH)
- Serum urea
- Liver function tests
- Chest X-ray or computed tomography (CT) scan of the chest
- CT scan of the head
Diagnostic Approach(Figure)
Management/ Treatment
Treatment of hyponatraemia depends upon the degree of hyponatraemia, duration of hyponatraemia, severity of symptoms, and volume status.
Acute symptomatic hyponatraemia
- Severely symptomatic hyponatraemia: Administer 3% sodium chloride; 100 mL intravenous (IV) bolus (repeat up to twice if symptoms persist).
- Mild to moderately symptomatic hyponatraemia: 3% Sodium chloride, slow infusion (use sodium deficit formula to calculate the infusion rate but recalculate rate with frequent sodium monitoring).
Chronic asymptomatic hyponatraemia
- Hypovolemic hyponatraemia: Isotonic fluids administration and holding of any diuretics.
- Hypervolemic hyponatraemia: Treat underlying condition, restrict salt and fluids, and administer loop diuretics.
- Euvolemic hyponatraemia: Fluid restriction to less than 1 litre per day.
Drugs
Selective vasopressin 2 receptor antagonists are being used recently. They increase the excretion of water in the kidneys without affecting sodium, thereby increasing serum sodium levels. These medications are used in patients with euvolemic and hypervolemic conditions (except liver failure) if the above measure does not help.
The goal of correction: Correct sodium by no more than 10 mEq/L to 12 mEq/L in any 24 hours.
Risk factors for osmotic demyelination syndrome (ODS): Hypokalemia, liver disease, malnutrition, alcoholism.
Complications
If left untreated or inadequately treated, patients with hyponatraemia can develop rhabdomyolysis, altered mental status, seizures, and even coma. Rapid correction of chronic hyponatraemia (greater than 10 mEq/L to 12 mEq/L of sodium in 24 hrs) can lead to osmotic demyelination syndrome.
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr Bhavin Mandowara is a practising nephrologist at Zydus Hospital, Ahmedabad.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries