Ankylosing spondylitis: How to treat?
M3 India Newsdesk Feb 11, 2022
Described here is the clinical and radiological criteria for diagnosis and the latest treatment guidelines for active and stable ankylosing spondylitis (AS).
New imaging techniques and therapies have substantially changed the management of ankylosing spondylitis (AS) disease in the past decade. Whether inhibition of radiographic progression and structural damage can be reached with available drugs is as yet unclear.
Furthermore, treatment with non-steroidal anti-inflammatory agents and physiotherapy remains an important approach to the long-term management of patients with ankylosing spondylitis. The new treatment options with tumour necrosis factor blockers seems a breakthrough for patients refractory to conventional treatment.
It is also important to recognise the strong correlation between the prevalence of HLA-B27 and AS in any given population. One must not forget that most individuals who test positive for HLA-B27 are healthy. Non–HLA-B27 genetic and environmental factors have an important role in the development and progression of this disease.
Clinical features
The primary clinical features of AS include inflammatory back pain caused by sacroiliitis, inflammation at other locations in the axial skeleton, peripheral arthritis, enthesitis, and anterior uveitis.
- Structural changes are caused mainly by osteoproliferation rather than osteodestruction.
- Syndesmophytes and ankylosis are the most significant characteristic features.
- The characteristic symptoms are low-back pain, buttock pain, limited spinal mobility, hip pain, shoulder pain, peripheral arthritis, and enthesitis.
- Neurological symptoms can occur with cord or spinal nerve compression resulting from several complications.
- Vertebral fractures can develop in patients with ankylosed spines with minimal or no traumatic injury. The most common fracture site is the C5–6 interspace.
- A clinically significant atlantoaxial subluxation can occur in up to 21% of patients with AS and can lead to spinal cord compression.
- Cauda equina syndrome is a rare complication of longstanding AS. It includes inflammation, arachnoiditis, mechanical stretching, compression of the nerve roots, demyelination, and ischaemia.
Clinical and radiological criteria for diagnosis
The diagnosis of AS is made from a combination of clinical features and evidence of sacroiliitis by some imaging techniques defined by the 1984 Modified New York Criteria.
The clinical criteria include:
- Low-back pain and stiffness of 3 months’ duration that improves with exercise but is not relieved by rest.
- Limitation of motion of the lumbar spine in both the sagittal and frontal (coronal) planes.
- Limitation of chest expansion relative to normal values corrected for age and sex.
The radiological criteria
- Sacroiliitis Grade 2 or higher bilaterally
- Grade 3 or higher unilaterally
The radiographic grading of sacroiliitis consists of 5 grades:
- Grade 0 is a normal spine.
- Grade 1 indicates suspicious changes.
- Grade 2 indicates sclerosis with some erosion.
- Grade 3 indicates severe erosions, pseudodilatation of the joint space, and partial ankylosis.
- Grade 4 denotes complete ankylosis.
Definite AS is present when one radiological criterion is associated with at least one clinical criterion. Probable AS is considered if there are 3 clinical criteria present or radiologic criteria exist with no signs or symptoms to satisfy the clinical criteria.
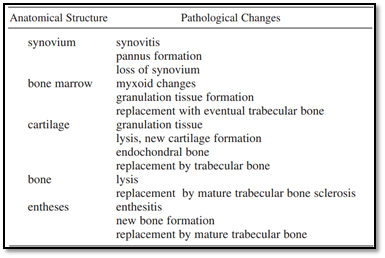
Pathological changes occurring in the joints eventually leading to AS
Based on new evidence and an expert consensus, the American College of Rheumatology (ACR), the Spondylitis Association of America, and the Spondyloarthritis Research and Treatment Network released updated recommendations for the treatment of AS in 2019.
Recommendations for the treatment of active AS
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs)- ACR strongly recommends that patients with active AS receive treatment with NSAIDs over no treatment with NSAIDs and no preferred choice of NSAIDs is recommended.
- Sulfasalazine, Methotrexate, Tofacitinib- Regardless of NSAID treatment, ACR conditionally recommends that adults with active AS be treated with sulfasalazine, methotrexate, or tofacitinib over no treatment; sulfasalazine and methotrexate should only be considered in patients with prominent peripheral arthritis or when tumour necrosis factor inhibitors (TNFi) are not available.
- Secukinumab, Ixekizumab- Despite treatment with NSAIDs, ACR strongly recommends treatment with secukinumab or ixekizumab over no treatment and conditionally recommends treatment with secukinumab or ixekizumab over treatment with tofacitinib.
- TNFi
- Despite treatment with NSAIDs, ACR strongly recommends treatment with TNFi over no treatment with TNFi and conditionally recommends TNFi over treatment with tofacitinib, secukinumab, or ixekizumab, no particular TNFi is recommended as the preferred choice.
- Adults with active AS who have contraindications to TNFi should conditionally receive treatment with secukinumab or ixekizumab over treatment with sulfasalazine, methotrexate, or tofacitinib. Secukinumab or ixekizumab are also conditionally recommended overtreatment with a different TNFi in patients with primary nonresponse to TNFi.
- Glucocorticoids- ACR strongly recommends against treatment with systemic glucocorticoids. In adults with active sacroiliitis or stable axial disease with active enthesitis or peripheral arthritis, treatment with locally administered parenteral glucocorticoids are conditionally recommended over no treatment with local glucocorticoids. Peritendon injections of Achilles, patellar, and quadriceps tendons should be avoided.
- Physical therapy- Physical therapy is strongly recommended over no physical therapy in patients with active AS. ACR recommends active interventions (supervised exercise) over passive interventions (massage, ultrasound, heat), and land-based physical therapy over aquatic therapy interventions.
Recommendations for the treatment of stable AS
- NSAIDs- In patients with stable AS, ACR conditionally recommends on-demand treatment with NSAIDs over continuous treatment with NSAIDs, no preferred choice of NSAIDs is recommended.
- TNFi- In adults receiving treatment with TNFi and NSAIDs, ACR conditionally recommends continuing with TNFi alone over continuing both treatments. Similarly, for patients receiving TNFi and conventional synthetic antirheumatic drugs, continuing with TNFi alone is recommended. ACR strongly recommends that adults treated with an originator TNFi continue with it rather than switching to the originator TNFi’s biosimilar.
- Biologics- In adults with stable AS who receive treatment with a biologic, ACR conditionally recommends against discontinuation or tapering of the biologic dose as a standard of care.
- Physical therapy- Treatment with physical therapy is strongly recommended over no physical therapy in patients with stable AS.
Recommendations for adults with active or stable AS
- ACR conditionally recommends against concomitant treatment with TNFi and low-dose methotrexate in adults with active or stable AS.
- Unsupervised back exercises are conditionally advised. However, spinal manipulation is strongly recommended in patients with spinal fusion or spinal osteoporosis.
- Fall evaluation and counselling are conditionally recommended for all adults with AS, along with participation in formal group or individual self-management education.
- Total hip arthroplasty is strongly recommended over no surgical treatment in patients with advanced hip arthritis, but ACR recommends against elective spinal osteotomy in adults with severe kyphosis.
Disease activity assessment
ACR recommends to clinicians the use of a validated AS disease activity measure at regular intervals for monitoring disease activity, and conditionally recommends the regular monitoring of C-reactive protein (CRP) or erythrocyte sedimentation rate (ESR) concentrations over usual care without CRP or ESR monitoring.
Imaging
ACR conditionally recommends obtaining a spinal or pelvis MRI to assess disease activity in adults with AS or non-radiographic axial SpA being treated with a biologic and for whom disease activity is unclear. In adults with stable AS or non-radiographic axial SpA activity, a spinal or pelvic MRI is conditionally recommended to confirm disease inactivity.
In patients with active or stable AS or non-radiographic axial SpA on any treatment, ACR conditionally recommends against obtaining repeat spine radiographs at regular intervals as a standard of care.
Screening
In adults with AS, ACR conditionally recommends screening for osteopenia/osteoporosis with a dual x-ray absorptiometry (DXA) scan over no screening; in patients with spinal fusion or syndesmophytes, screening for osteoporosis/osteopenia with a DXA scan is conditionally recommended for the spine as well as the hips, compared with obtaining a DXA scan of only the hip or other non-spine sites.
In a study on the Indian population, the male/female ratio of AS was 5:1. The mean age of onset of symptoms and diagnosis was 23.6 and 32.5 years, respectively. Females had similar spinal indices and radiological damage as their male counterparts.
However, they had more common extra-articular manifestations and root joint involvement. The majority of patients consisted of Adult-Onset AS (78.5%) and was clinically similar to Juvenile-Onset AS. One or more peripheral joints were involved in 65.7% of patients, affecting predominantly the lower extremity (90.6%, knee 47.1%, and ankle 35.7%) in an asymmetrical pattern (78%).
Conclusion
New imaging techniques and therapies have substantially changed the management of this disease in the past decade. Whether inhibition of radiographic progression and structural damage can be reached with available drugs is as yet unclear. Furthermore, treatment with non-steroidal anti-inflammatory agents and physiotherapy remains an important approach to the long-term management of patients with ankylosing spondylitis. The new treatment options with tumour necrosis factor blockers seem a breakthrough for patients refractory to conventional treatment.
Click here to see references
Disclaimer- The views and opinions expressed in this article are those of the author's and do not necessarily reflect the official policy or position of M3 India.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries