Anaesthetic Management of TURP
M3 India Newsdesk Jan 10, 2025
In order to improve urine flow, a surgical technique called transurethral resection of the prostate (TURP) removes tissue from the prostate. This article presents a case report of TURP Syndrome. It also discusses the complications and management of this condition.
Case report
A 58-year-old male presented with complaints of increased frequency, urgency, and urinary retention for the past six months. He has been a known case of hypertension for five years and is on regular treatment with Tab—amlodipine 5 mg BD. He also has a history of asthma for the past ten years with seasonal exacerbations, regularly managed with a metered-dose inhaler (MDI) containing Formoterol fumarate and Budesonide. His last episode of exacerbation occurred two years ago.
Clinical examination
The patient was conscious and oriented.
- Height: 165 cm
- Weight: 58 kg
- Pulse rate: 88 bpm
- Blood Pressure: 140/80 mmHg
- Auscultation: Normal; chest was clear
- Airway examination: Normal (MPG 3, TMJ > 6.5 cm, adequate mouth opening)
- Spine examination: Normal
- Dentition: No loose or missing teeth
Investigations
- Haemoglobin: 13.2 g/dL
- WBC count: 8,900/cumm
- Platelet count: 2.97 Lakhs/cumm
- Blood Urea: 18 mg/dL
- Serum Creatinine: 0.8 mg/dL
- Electrolytes: Na 139, K 4, Cl 102
- Random Blood Sugar: 132 mg%
- PT: 15 seconds
- INR: 1.1
- Viral Serology Markers: Negative
- Chest X-ray and ECG: Normal
- Echocardiography: Concentric LVH, EF 63%, no regional wall motion abnormality
- Ultrasound: Prostate gland size – 45 ml
- Cardiologist Opinion: Moderate surgical risk
- Pulmonologist Recommendation: Pre- and postoperative nebulisation with Levosalbutamol + Ipratropium Bromide and Budesonide solutions.
Preoperative Medication: Tab. Alprazolam 0.25 mg was administered the night before surgery.
Management
- On the day of surgery, the patient’s morning dose of antihypertensive medication and nebulisation were administered.
- Standard ASA monitors were attached in the operating room, and an 18G IV cannula was inserted in the left hand. NS infusion was started.
- HR: 97/min
- BP: 144/82 mmHg
- SpO2: 97% on room air
The anaesthetic plan was to proceed with spinal anaesthesia.
- In a sitting position, under strict aseptic precautions, 2.8 ml of hyperbaric 0.5% bupivacaine was administered at the L3-L4 interspace.
- After achieving a sensory block up to T10, the surgery commenced.
- Hypotension during the procedure was managed with 6 mg boluses of Inj. Ephedrine.
- An air warmer was used to prevent hypothermia.
Intraoperative details:
- Total surgery duration: 45 minutes
- Resection time: 30 minutes
- Irrigation fluid: 1.5% Glycine
- Estimated blood loss: 200 ml
Postoperatively, the patient was shifted to the recovery room, where vitals were monitored. Two hours later, the spinal block regressed to T12, and the patient was transferred to the postoperative ward.
Discussion
The prostate has a rich blood supply and venous drainage through large, thin-walled sinuses adjacent to the capsule. Pain signals from the prostate are carried by sacral nerves (S2-S4), while the sensation of bladder distension is transmitted by sympathetic nerves (T11-L2).
Surgical resection is performed via a modified cystoscope using resection and coagulation currents in the lithotomy position. Continuous irrigation is essential to distend the bladder, wash away blood, and remove dissected prostatic tissue.
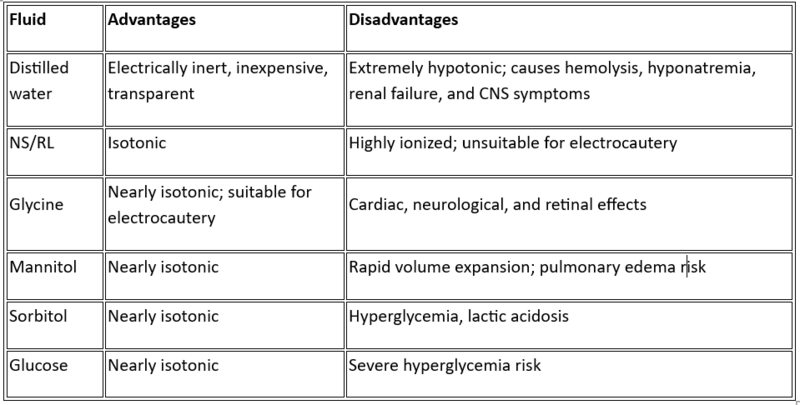
Ideal Irrigation Fluid
Irrigation fluids should ideally be:
- Transparent
- Electrically non-conductive
- Isotonic
- Non-toxic and non-hemolytic
- Easy to sterilise
- Inexpensive
- Non-metabolised and easily excreted
No solution meets all these criteria.
Anesthesia technique
- Spinal anaesthesia: Preferred as it provides adequate pelvic floor and perineal relaxation, and allows for early recognition of complications like TURP syndrome. A sensory block at T10 interrupts sensory transmission from the prostate and bladder neck, eliminating discomfort from bladder distension.
- Epidural anaesthesia: Less favourable due to incomplete blockade of sacral nerves.
- General anaesthesia: Masks symptoms of severe complications and is used only when regional anaesthesia is contraindicated.
Complications of TURP
- Absorption of irrigation fluid
- Volume overload, hyponatremia, hypoosmolarity
- Glycine or ammonia toxicity
- Bladder perforation
- Transient bacteremia/septicemia
- Hypothermia
- Bleeding or coagulopathy
Signs and symptoms of TURP syndrome
- Cardiovascular/Respiratory: Hypertension, arrhythmias, heart failure, pulmonary edema, myocardial infarction.
- CNS: Agitation, confusion, seizures, coma, visual disturbances.
- Metabolic: Hyponatremia, hyperammonemia.
- Other: Hypoosmolality, hemolysis, acute renal failure.
Management of TURP syndrome
- Recognise and terminate the procedure immediately.
- Provide symptomatic management, including supplemental oxygen, ventilation, and cardiovascular support.
- Obtain blood samples for electrolytes, glucose, and arterial blood gases, and perform a 12-lead ECG.
- Treat hyponatremia based on severity:
- Na > 120 mEq/L: Fluid restriction and diuretics (furosemide)
- Na < 120 mEq/L: IV hypertonic saline (3%) under close monitoring
- Avoid rapid correction of sodium to prevent central pontine myelinolysis or cerebral oedema.
Take-home messages
- Preoperative optimisation of cardiac status is crucial.
- Spinal anaesthesia with a T10 block enables early recognition of TURP syndrome.
- General anaesthesia may obscure complications.
- Epidural anaesthesia may spare sacral nerves, resulting in incomplete analgesia.
- A high index of suspicion for TURP syndrome is essential.
- Correct hyponatremia cautiously and avoid rapid correction.
- Multidisciplinary coordination between surgical, anaesthetic, and nursing teams ensures the best patient outcomes.
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr N Chinna Siddeswarappa is an Assistant professor (Anaesthesiology dept.) at Meenakshi Medical College Hospital And Research Institute, Kanchipuram.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries