Anterior Cruciate Ligament Injuries (ACL): A Paradigm Shift In The Treatment: Dr Suresh Dargan
M3 India Newsdesk Aug 22, 2022
Anterior cruciate ligament (ACL) injuries are one of the most common knee injuries in sports. In this article, the author elaborates on the history, treatment modalities and types of grafts that are implemented for ACL injuries.
ACL injuries
Nothing is more controversial than the management of ACL injuries in the field of knee trauma. Treatment of ACL injuries has a very fascinating evolutionary history based on continuous progressive ideas, scientific research and clinical evidence.
The history of an ACL surgery can be traced as far back as Egyptian times. Improved anatomical, physiological and biomechanical knowledge has led progressively to a better understanding of ACL ruptures evolving from the initial conservative cast immobilisation treatment of the past centuries to surgical repair and reconstruction.
Primary open repair of the ACL was the standard surgical technique for ACL ruptures until the 1980s followed by arthroscopic autograft ACL reconstruction. Recently there has been a resurgence of interest in ACL preservation rather than in ACL reconstruction. With a better understanding of the pathophysiology of healing of torn ACL, advancements in MRI quality, regenerative medicine, tissue engineering capabilities, various arthroscopic techniques and instrumentation, there is going to be a paradigm shift in the management of these injuries from ACL reconstruction to bio-enhanced repair and even to non-operative conservative treatment.
Treatment modalities
The primary goal of the treatment is to restore normal knee kinematics, to provide a pain-free stable knee and to provide an early return to the previous level of function. Treatment of ACL injuries depends upon various factors like age, gender, duration of injury, anatomical level of tear, the extent of tear, activity level of patient and associated injuries.
1. Non-operative treatment
It includes a short period of immobilisation, bracing, a progressive rehabilitation programme, and regular follow-up evaluations. It is indicated in the following patients:
- With partial tears and no instability symptoms.
- With complete tears and no symptoms of knee instability during low-demand sports who are willing to give up high-demand sports.
- Who do light manual work or live sedentary lifestyles.
- Whose growth plates are still open (children).
2. Operative Methods
a) Primary Repair
It is performed by re-approximating the ruptured ends of the native ACL with the use of sutures or suture anchors. It was first described by Mayo-Robson in 1895. Outcomes of open primary repair were good to excellent and did not deteriorate when this technique was selectively performed in patients with proximal ACL tears, whereas primary repair led to disappointing and unpredictable results in patients with mid-substance tears.
b) ACL reconstruction
It is done by debriding the torn ends of the native ACL to reconstitute the anatomy and function of the native ACL using grafts. It is indicated in cases of complete mid-substance ACL tear with knee instability, associated with tears of other ligaments and menisci, especially in young individuals and athletes who aim to return to high-level sporting activities.
ACL reconstruction has evolved considerably over the past 30 years. This has largely been due to a better understanding of ACL anatomy and in particular a precise description of the femoral and tibial insertions of its two bundles. In the 1980s, the gold standard was anteromedial bundle reconstruction using the middle third of the patellar ligament. Insufficient control of rotational laxity led to the development of double bundle ACL reconstruction.
Various problems related to this surgery are anterior knee pain, kneeling pain, hamstring weakness, rotatory instability, re-rupture, extensive rehabilitation period, development of osteoarthritis and clinical failure.
Types of grafts
1. Autograft
- Bone patella tendon bone (BPTB) autograft is classically harvested from the middle third of the patellar tendon. It produces a consistent graft diameter of around 10 mm and contains bone plugs from the patella and tibia at either end of the graft that facilitates bone-to-bone healing within the bony graft tunnel.
- Hamstring tendon (HT) autograft is harvested from the semitendinosus and/or gracilis tendon to yield variable sizes and constructs. In contrast to the BPTB autograft, the HT autograft is a soft tissue graft without bone plugs, therefore relying on soft tissue healing in bony tunnels, which may occur more slowly and is weaker compared to bone-to-bone healing.
- Quadriceps tendon (QT) autografts have demonstrated good strength, low donor-site morbidity, and reliable long-term outcomes.
Advantages of autografts are lower re-rupture rate in younger, high-activity patients, no risk of rejection or disease transmission and faster incorporation.
2. Allograft
The graft is taken from a donor (a deceased donor in cases of ligament transplants). The advantages include less post-operative pain, smaller scars, easier rehabilitation and no graft harvest site issues. Disadvantages include graft availability, higher cost, lower strength and more significantly, disease transmission risk and graft rejection. Current evidence supports its use in specific circumstances such as multi-ligament knee reconstruction, inadequate autograft tissue, or in older, less active populations.
3. Artificial grafts
These are fibres made of materials such as carbon fibre, polypropylene, Dacron and polyester. They have serious drawbacks- cross-infections, immunological responses, breakage, debris dispersion leading to synovitis, chronic effusions, recurrent instability and knee osteoarthritis.
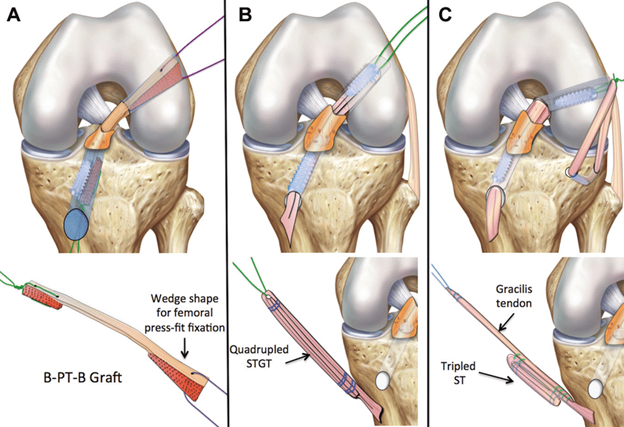
Figure:1
Anterior cruciate ligament reconstruction with an (A) bone-patellar tendon-bone (B-PT-B) graft, (B) quadrupled Semitendinosus Gracilis tendon (STGT) graft, and (C) hamstring tendon graft combined with anterolateral ligament reconstruction.
4. Repair with bioaugmentation- A new paradigm in ACL injuries
Bioaugmentation is a technique of using an extracellular matrix, a collagen-based scaffold and autologous blood for repairing torn ACL. Other bio-augmentation techniques include:
- Growth factors, platelet-rich plasma (PRP) and fibrin clot.
- Mesenchymal stem cells (MSC)
- Autologous tissue.
- Various pharmaceuticals (matrix metalloproteinase-inhibitor alpha-2-macroglobulin bisphosphonates)
- Biophysical methods (hyperbaric oxygen, low-intensity pulsed ultrasound, extracorporeal shockwave therapy)
- Biomaterials (fixation methods and biological coatings)
- Gene therapy.
These bioaugmentation techniques can be used in conjunction with unrepaired partial tears, primary repair or in the reconstruction of ACL to ensure the ligamentisation.
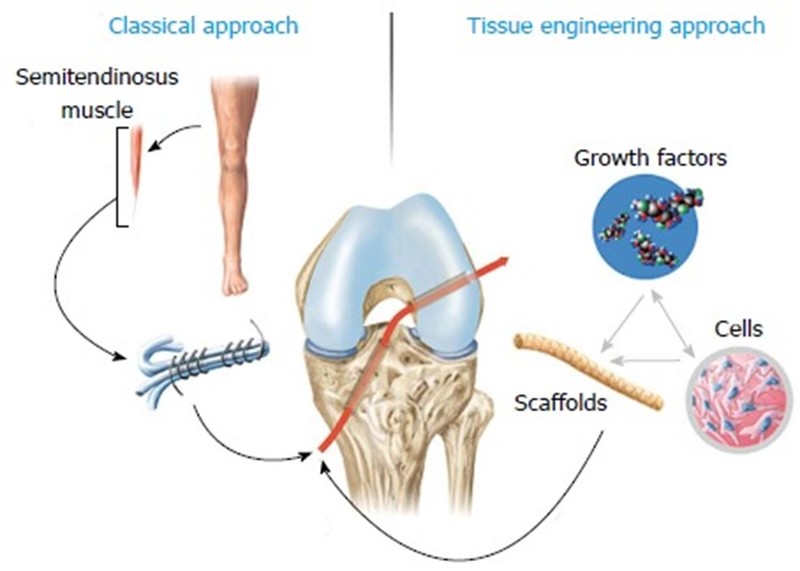
Figure:2
Comparison of classical approach to tissue engineering approach in anterior cruciate ligament surgery.
5. Novel primary ACL repair
Primary ACL repair may be considered in cases of proximal tears with good tissue quality, whereas ACLR remains the preferred technique in non-proximal tears, with poor tissue quality and with associated ligamentous injuries. This method allows you to re-attach broken ligaments in their original position. Primary ACL repair techniques have some advantages over autograft ACL reconstruction i.e. maintenance of proprioception, less invasiveness, regain of early range of motion, restoration of native kinematics, avoidance of donor site morbidity and prevention of osteoarthritis. In addition, standard ACL reconstruction can be easily performed if primary ACL repair fails, while revision surgery for failed ACL reconstruction is much more complex.
Types of primary ACL repair techniques
- Suture anchor repair (SAR) of the ACL
- Repair with dynamic intraligamentary stabilisation (DIS): It uses a threaded sleeve with a preloaded spring in the tibia, from which a 1.8 mm polythethylene wire is passed through torn ACL and made exit out lateral distal femur, where it is secured with a button, associated to femoral micro fracturing.
- Internal brace ligament augmentation (IBLA): It is based on the use of a 2.5 mm polythethylene tape to bridge from the anatomical attachments of the mid-bundle positions of the ACL on both the femur and the tibia associated with femoral micro fracturing. Studies have demonstrated improved stability and graft protection because IBLA works as a load-sharing device, still allowing the graft to see enough stress to undergo ligamentisation.
- Bridge-enhanced ACL repair (BEAR) uses bio-scaffold.
Conclusion
The management of ACL injuries is one of the most extensively researched subjects in the field of orthopaedic trauma. ACL reconstruction using autografts like hamstring tendons, patellar tendons or quadriceps tendons is the current gold standard for treating ACL injuries despite inherent challenges. ACL preservation seems to be an ideal option to restore native knee kinematics and proprioceptive function.
Old is becoming new again. ACL repair rather than reconstruction, first pioneered in the nineteenth century is being reinvented. Recent studies indicate the shift of paradigm of treatment of ACL injuries from reconstruction to repair or even conservative management in properly selected patients.
This is been made possible due to the advancements in molecular biology, gene therapy, and tissue engineering in conjunction with robotic technology and computer-assisted surgery. Nevertheless, more randomised controlled trials comparing ACL repair with ACL reconstruction are needed.
Click here to see references
Disclaimer- The views and opinions expressed in this article are those of the author's and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr Suresh Dargan is a senior consultant (orthopaedics) in Dwarka, New Delhi.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries