A Treatment Guide to Various Infections For Ophthalmic Emergencies
M3 India Newsdesk Oct 28, 2022
In this second part of the ophthalmic emergencies article, practitioners will get guidance on some more vision-threatening disorders along with their presentation, examination, and management.
In the previous part we have covered eye injuries, now we will be aiming at the diseases characterised by eye inflammation.
Preseptal versus Orbital Cellulitis
What is orbital cellulitis?
Orbital cellulitis, also known as post-septal cellulitis, is more invasive and affects orbital soft tissues that extend beyond the orbital septum, including fat, connective tissues, and muscles.
Causes:
- Cellulitis of the periorbital or pre-septal region occurs as a consequence of the progression of rhinosinusitis, infection, superficial skin infection, or facial trauma.
- It is characterised by inflammation of the eyelids and soft tissues just anterior to the orbital septum.
It is critical to differentiate the two forms of cellulitis since care varies according to diagnosis:
- Orbital cellulitis may be vision- and life-threatening in rare instances owing to orbital compartment syndrome, cavernous sinus thrombosis, meningitis, or brain abscess.
- Pre-septal cellulitis is characterised by periorbital erythema, oedema, and eyelid swelling.
- However, there is no effect on vision, eye movement, or intraocular pressure.
- In addition to the periorbital erythema and swelling observed with pre-septal cellulitis, orbital cellulitis may manifest with conjunctival injection and oedema, proptosis, ophthalmoplegia with diplopia, discomfort and impaired EOM movement, and diminished vision.
- Systemic symptoms such as fever and malaise are more often linked with orbital cellulitis, however, they may occur in pre-septal cellulitis on occasion.
Diagnosis:
- A full ophthalmologic examination is advised for both entities, including visual acuity testing, pupillary response testing, eye motility testing, and tonometry. However, in circumstances when the two are difficult to identify, an orbital and sinus CT scan is recommended.
- In individuals with orbital cellulitis, inflammation of the EOM, fat stranding, and anterior globe displacement may be seen on a CT scan.
- If orbital cellulitis is identified, the patient should have an immediate ophthalmologic assessment to rule out the development of orbital compartment syndrome, optic neuropathy, or abscesses, all of which would need an emergent lateral canthotomy/cantholysis or surgical drainage of the abscess.
Management:
- Antibiotic therapy should address Staphylococcus, Streptococcus, and anaerobic bacteria.
- Pre-septal cellulitis is treatable on an outpatient basis with trimethoprim-sulfamethoxazole or clindamycin + amoxicillin, amoxicillin-clavulanic acid, or cefdinir.
- The majority of patients with orbital cellulitis necessitate hospitalisation, and initial therapy with intravenous vancomycin plus cefotaxime or ceftriaxone and metronidazole or clindamycin should be started until cerebral involvement or sinusitis is ruled out.
- Response to therapy should be visible within 24 to 48 hours after initiating proper therapy, with treatment continuing for at least 2 to 3 weeks or until all indications of cellulitis have disappeared.
- When a patient with pre-septal cellulitis deteriorates or does not recover within 24 to 48 hours of therapy, a CT scan and probable hospitalisation are recommended to rule out orbital cellulitis and sequelae.

Endophthalmitis
Endophthalmitis is an infection of the vitreous, retina, choroid, and/or anterior chamber of the eye caused by bacteria or fungus.
Cause:
- It is most often caused by foreign organisms introduced during recent operations such as intravitreal/intraocular injections and eye surgery.
- Endogenous endophthalmitis is also a possibility as a result of an organism being seeded via the bloodstream.
- These are medical crises, and any delay in treatment may result in irreversible eyesight loss.
Diagnosis:
- Patients often appear with fast-escalating discomfort, red eye, ocular discharge, and vision loss within 1 week following a recent ocular operation.
- The examination may reveal swelling of the eyelids, conjunctival or corneal oedema, or hypopyon (collection of inflammatory cells in the anterior chamber of the eye).
Management:
Urgent ophthalmology consultation is recommended to allow for a more thorough ophthalmologic examination, the collection of intravitreal samples for culture and speciation, and the administration of intravitreal antibiotics.

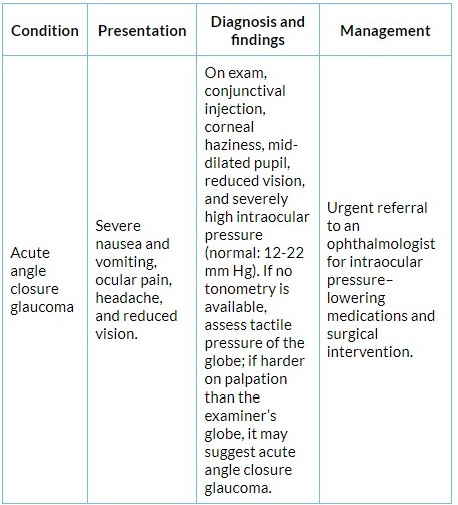
Acute angle closure glaucoma
Causes:
- Because of a reduction in an aqueous outflow from the posterior to the anterior chamber, angle closure glaucoma is caused by a narrowing of the anterior chamber angle.
- Because of the increased intraocular pressure caused by this pressure difference, structural changes occur in the iris and trabecular meshwork.
- Women, individuals over the age of 50, and those with a family history of angle closure glaucoma are more likely to develop the illness.
- Affected patients may report severe nausea/vomiting, ocular discomfort, impaired vision, and headache, all of which suggest that a migraine is a possibility.
Diagnosis:
Monocular symptoms, conjunctival injection, corneal haziness owing to oedema, a mid-dilated pupil, and an abrupt loss of vision might help differentiate this condition from mimickers.
Management:
- A prompt referral to an ophthalmologist is suggested to allow for medication or surgical treatment.
- The intraocular pressure is measured and gonioscopy, a study of the angle between the eye and cornea, is performed to confirm the diagnosis.
This is part 2 of the article. Please stay tuned for the next part of this series. Click here to read the previous parts-A guide to ophthalmic emergencies
Click here to see references
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr Monish Raut is a practising super specialist from New Delhi.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries