Krait & Cobra bite: Treatment protocol & Management- Dr. H Bawaskar
M3 India Newsdesk Dec 21, 2018
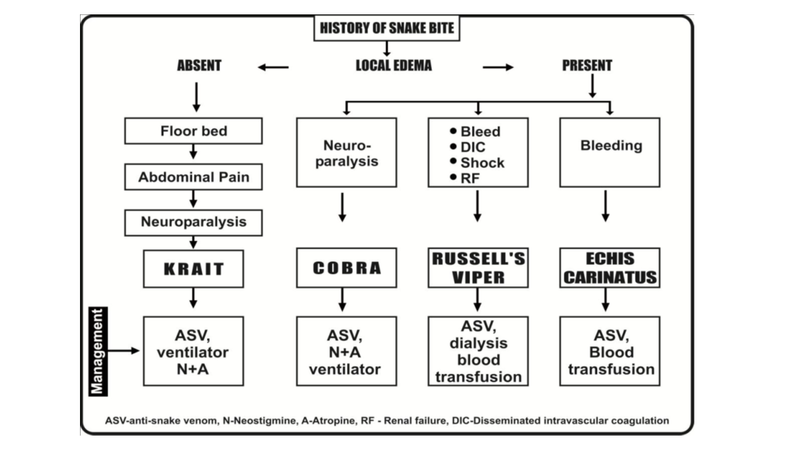
Dr. H. Bawaskar, a physician known for his extensive research in snake bites discusses the diagnosis of different types of snake bites and the corresponding management for each. Here he covers Indian Krait and Cobra bites.

ATTENTION: The images in this article contain pictures of snakes and patient presentations which some people may find offensive or disturbing. Viewer discretion is advised.
Snake-bite poisoning is an occupational hazard and a common accident reported among farmers, villagers, labourers, hunters, trekkers, snake rescuers, migrating population like shepherds, scientists working with snakes for milking, and persons who take care of snakes in snake parks are more prone for snake bite accidents. It is a common accident reported in tropical and subtropical countries.
Snake bites evoke a time-limiting, life-threatening emergency. More than 20,00,000 snake bite incidences are reported in India and of these >46,900 people die each year, which means that every hour 5 patients lose their lives to snake bites*. This is just a tip of the iceberg as a majority of the times, victims die at home by being attended to by a Mantrik or on the way to a hospital, and the cases remain unreported. Lack of knowledge, improper training regarding early reorganisation of venomous snake bites and rapid intervention may add to mortality and morbidity.
Irrespective of high fatality, snake bites remain totally neglected in rural India though they are recognized in the type A category of neglected tropical diseases by WHO. It is a surprise to note, and snakebite poisoning is seldom mentioned as a priority for health research in a developing country like India.
Availability of snake-venom antigen detection kits (ELISA), mono-specific or antivenom producers in India should be encouraged to prepare anti-venom from venom obtained from snakes caught from relevant areas of the country. Recently, the high incidence of snake bites was attributed to electric load shading for more than 12 hours in rural areas. The government should provide all facilities including anti-snake venom (ASV), life support gadgets like ventilators and emergency treatment rather than giving compensation to the relatives of patients who die from snake bites.
India's poisonous snakes
Of more than the 3,000 known species of snakes, only about 300 are venomous and there are about 216 species of snakes identifiable in India, of which 52 are known to be poisonous. The major families of poisonous snakes in India are:
- Elapid which includes common cobra (Naja naja), king cobra and common krait (Bungarus caerulus, banded krait, sind krait)
- Viperidae includes Russell’s viper, Echis carinatus (saw-scaled or carpet viper) and pit viper
- Hydrophidae (sea snakes)
Venom secretion in all venomous snakes appears to vary in seasons more in warmer months with high morbidity and fatality. The darker the snake, the more venom it secretes.
Biochemistry, physiology, and pathology of envenoming
Most snakes inject 10% of the available venom in single strike except Russell’s viper injects 75% of stored venom in one bite due to big long sharp curved fangs.
Snake venom is a cocktail of 20 or more components including proteins, enzymes, non-enzymatic polypeptide toxins, non-toxic nerve growth factors, hyaluronidase, metals, lipids, free amino acids, nucleotides carbohydrates, biogenic amines and various activators and inactivates of physiological processes. Venom from both types contains acetylcholine esterase, phospholipase B and glycerophosphatase.
Krait venom
Krait venom is ten times more lethal than the cobra, victim report too late due to delayed clinical manifestations.

Krait Bungarus caeruleus
Krait is nocturnal in habit. Its fangs are small size like that of a 24-size needle. It injects the venom deep into the skin. Though the venom is of small molecular size, it is absorbed slowly as skin has poor circulation and reflexes are blunted during sleep. Beta bungarotoxin in the krait venom bears similarity to botulinum toxin. Common Indian Krait venom contains both presynaptic beta bungarotoxin and alfa bungarotoxin.
- Mode of action: The toxins initially release acetylcholine at the nerve endings at the neuromuscular junction and then damage it subsequently preventing the release of acetylcholine and receptors are damaged and destroyed, the cause of resistance to anti-cholinesterase.
- Symptoms: Initial release of acetylcholine results in autonomic nerve stimulation, in addition, to release of cholecystokinin explained by acute abdominal pain, vomiting, staring look, blurring of vision, gooseflesh, salivation, hypertension, pulmonary oedema.
Clinical manifestations of Common Krait bite
The common krait is regarded as the most dangerous species of venomous snake in the Indian subcontinent. Most bites occur during the cooler months of June to December, when snakes may, during the course of their hunting activity, linger on a person’s bedding to take advantage of the warmth.
Krait bite patterns
| Patients | Total | Percentage |
| Male | 79 | 56 |
| Female | 62 | 34 |
| Approximate Time of Bite | Total | Percentage |
| 6 pm to 12 am | 34 | 24.11 |
| 12 am to 5 am | 106 | 75.17 |
| Day bite | 1 | |
| Activity at the Time of Bite | Total | Percentage |
| Sleep | 140 | 99.29 |
| Activity | 1 | |
| Snake seen, killed and brought to the hospital | 42 | 29.78 |
| Saw the snake and confirmed by specimen and photographs | 19 | 13..47 |
| Site of Bite | Total | Percentage |
| Lower extremities | 43 | 30.49 |
| Upper extremities | 32 | 22.69 |
| Other parts | 28 (neck- 7, abdomen- 2, axial- 5, back- 6, chest- 3, ear- 5) | 19.85 |
| No history of bite | 38 | 26.95 |
Krait bite symptoms
| Signs & Symptoms | Total | Percentage |
| Pain in abdomen | 120 | 85.10 |
| Chest pain | 102 | 72.34 |
| Tenderness over abdominal and other muscles | 121 | 85.81 |
| Vomiting | 59 | 41.84 |
| Difficulty in deglutition | 110 | 78 |
| Sweating | 24 | 17.02 |
| Bilateral ptosis | 126 | 89.36 |
| Blurred vision | 72 | 51.06 |
| Suffocation | 86 | 60.99 |
| Ophthalmoplegia | 100 | 70.92 |
| Pooling of saliva | 52 | 38.87 |
| Hypertension | 23 | 16.31 |
| Hypotension | 5 | 3.58 |
| Bradycardia | 6 | 4.25 |
| Tachycardia | 3 | 2.12 |
| Pulmonary oedema | 4 | 2.83 |
| Quadriplegia | 42 | 29.78 |
| Neck drop | 47 | 33.33 |
| Respiratory depression | 50 | 35.46 |

Because of negligible or absent local manifestations, envenomation is neglected and falsely initially attributed to ant or rat bite or no bite at all.
The venom stimulates the autonomic nervous system within 20 to 30 minutes of the bite.
- The victim wakes up to transient abdominal colicky pain, vomiting (once or twice), and chest pain. Relatives and even an inexperienced doctor could neglect these vital symptoms by attributing them to indigestion or acidity or an acute attack of appendicitis and minimum T wave inversion due to hypoxia.
- Such a victim is then referred and admitted to the intensive coronary care unit. The tissues having a high concentration of acetylcholine receptors are affected earlier. The sphincter pupillae, elevator palpebral superior, neck muscles, bulbar, limbs, and at last the diaphragm and intercostal muscles are affected.
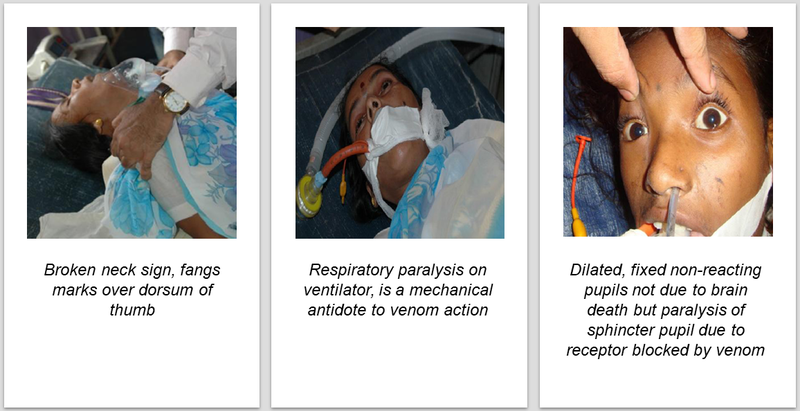
Clinical effects are seen within 30 minutes or sometimes too late in around 18 hours.
- Quadriplegia with aphasia and dilated pupils may be diagnosed as brain death or locked in syndrome [pseudo coma] or GB syndrome. The patient can communicate by flicker venom-induced paralysis of pupillary muscle resulting in non-reacting pupils, but this is not the sign of irreversible brain damage.
- After recovery, few patients have signs and symptoms of peripheral neuropathy.
- Many times, patients succumb to iatrogenic respiratory infection or adult respiratory distress syndrome.
At times, krait-bite victims even bring the killed snake but do not develop any clinical manifestations, local fangs marks without urticaria, indicated bite without envenoming or “dry bite”.
An inexperienced treating doctor may diagnose a krait bite envenoming even if a patient brings a specimen of wolf snake. To confirm or identify the venomous krait it is best to look at the tail which is covered by white bands till its end. This feature is absent in wolf snake (picture below), a non-venomous species which apparently looks like krait.

Management of Krait bite
First aid should be provided at home or place where the bite occurs
- If one succeeds to locate the bite site, the surface-deposited venom should be removed by a clean cloth or cotton.
- The bitten part should be kept below heart level.
- Crepe bandage should be used from the distal end of the bite site with the right amount of pressure so that one can easily put and remove the finger from underneath the bandage. The crepe bandage carries no benefit if the victim cannot reach the hospital within 30 minutes, and a delay of more than 4 hours is expected.
- The victim should not be allowed to walk.
- Mouth-to-mouth ventilation should be started to tide over the emergency.
Steps to be taken by the doctor are:
- Collect details and patient history, and patient activity at the time of the bite
- Initial clinical signs such as bulbar palsy, muscle power, tendon reflexes, respiratory rate, oxygen saturation, one-minute counting, pooling of saliva, broken neck sign should be noted in detail.
- Blood pressure and ECG changes should be monitored.
- Serum electrolytes and renal profiling should be done every few hours till clinical improvement is seen.
- On arrival 100 ml (10 vials) of anti-snake venom (ASV) should be added to 200 cc of normal saline and should be run over 30 to 50 minutes.
- One should sit by the side of the victim for early diagnosis and treatment of anaphylaxis.
Repetition of ASV: Within 30 minutes after the initial dose of ASV, if there is no improvement of neurological manifestations, one can repeat dose of ASV, but no more than a total of 20 vials of ASV should be administered. ASV only neutralizes circulating venom and it has no action once the venom is attached to the receptor site.
In krait bite there is a destruction of receptors, thus neurological manifestations may persist for weeks till there is a regeneration of receptors. At this stage administration of ASV is merely a waste.
Ventilation may be required if:
- Pooling of saliva in the victim is noticed
- Is unable to lift the neck from the pillow
- There is a reduction in SpO2 saturation
- Respiratory failure is noticed
- Abdominal-thoracic respiration occurs
If suffocation and signs of cerebral hypoxia occur:
- At the periphery, one can do entro tracheal intubation
- If this is not possible a laryngeal mask can be put directly over the larynx and ambu bag ventilation can be started
The last to recover is ptosis and the proximal muscles of lower limbs.
Anticholine esterase inhibitor (AChI)
Indian common krait venom contains both pre- and post-synaptic blockers. Whether the victim responds to AChI or not can be confirmed by placing an ice-filled glove finger over the eyelids. Hypothermia sensitizes the AChl receptors of acetylcholine. If there is a slight improvement in ptosis one can try AChI.
Severe uncontrolled hypertension
In krait bite, this is attributed to the blocked presynaptic receptors and unblocked post-synaptic receptors which release epinephrine into circulation. At times the victim may land up with acute myocardial failure with pulmonary oedema and need intravenous nitroglycerine drip and BIPAP ventilation. Severe hypertension with tachycardia and pulmonary oedema recover with nitroglycerine drip and non-invasive ventilation.
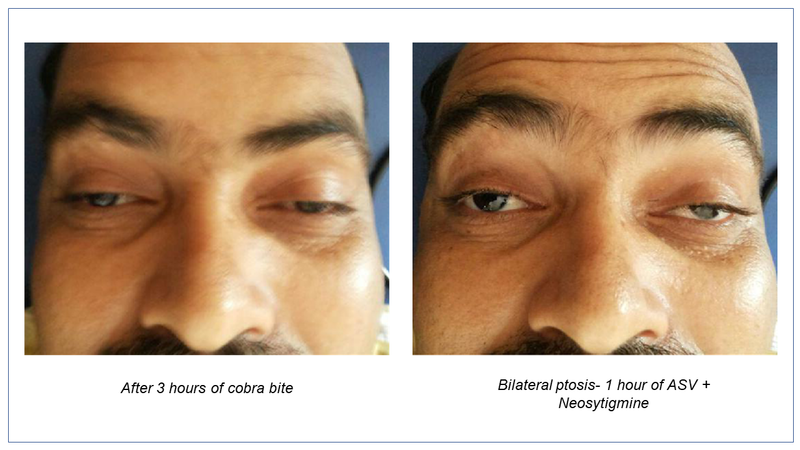
Cobra bite
Cobra venom is of smaller molecular size and rapidly absorbed into the circulation. The venom reversibly attaches to postsynaptic receptors. Absorption is further accelerated by the threat of death and liberated catecholamine and running can kill the victim within 8 minutes.
- Mode of action: Cobra venom binds specifically to the acetylcholine receptors, preventing the interaction between acetylcholine and receptors on postsynaptic membrane, thereby resulting in a neuromuscular blockade.
- Treatment: Administering appropriate antivenom ( in India polyvalent antivenom against krait, cobra, Russell’s viper and Echis) accelerates the dissociation of the toxin-receptor complexes and reverses paralysis.
- Cardiotoxin content of cobra venom has a direct action on skeletal, cardiac, smooth muscles, nerves and neuromuscular junction causing paralysis, circulatory, respiratory failure, cardiac arrhythmias, heart block and systolic cardiac arrest because of venom release causing calcium ions to move from the surface membrane to the myocardium.
Cobra bite tends to occur during the daytime when transportation is more readily available.
- Soon after the bite, the victim experiences severe pain at the bite site having fang marks. Fang marks are covered with blood clots. There is a rapid progression of swelling from the bitten part to the rest of the limb. Victims bitten by the hooded cobra may die of cardiac lethal ventricular arrhythmias or cardiogenic shock due to massive myocardial infarction.
- The skin at and around the bite site becomes ecchymosed.
- The victim subsequently develops tense blebs and massive damage of skin and subcutaneous tissue due to myocytolysis and huge non-healing ulcers.
- Later, the victim may develop stress-induced or ballooning cardiomyopathy as a result of massive liberation of endogenous catecholamine into circulation. This phenomenon, however, could be absent in children.
Management of cobra bite
First-aid that should be administered:
- The victim should not be allowed to walk or run, and the bitten part should be kept below heart level.
- No time should be wasted in using tourniquets. If a patient is found totally unconscious with no respiration mouth-to-mouth ventilation and chest compression should be tried.
Once the victim reaches the hospital:
- Administer ASV 100 ml (10 vials) by intravenous route; a maximum 20-25 vials can be used
- Begin artificial ventilation by ambu bag or ventilator
- Administer Neostigmine 50 µg/kg over the first hour and then 25 µg/kg in the next couple of hours preceded by atropine to counter the muscarinic action of AChI or 0.5 mg neostigmine half-hourly, preceded by atropine
- Prescribe local wound care of intravenous antibiotic, daily dressing, and plastic surgery if required

Local tissue damage requiring plastic surgery skin grafting
A majority of the victims recover within 24 hours and may require not more than 5-6 doses of AChI. In our experience, a victim declared as dead by a peripheral doctor only based on the absence of respiration and non-reacting pupils was recovered with artificial ventilation, CPR, and AChI.
*Source: Snakebite envenoming. Prevalance of snakebite envenoming.
In the upcoming articles, Dr. H Bawaskar discusses the treatment and management of victims reporting with Russell's viper and sea snake bites.
The writer, Dr. Himmatrao Bawaskar is a renowned Indian physician with publications in The Lancet. He has done extensive research in scorpion sting- diagnosis and treatment protocol.
Disclaimer- The views and opinions expressed in this article are those of the author's and do not necessarily reflect the official policy or position of M3 India.
The author did not accept any payment for the article.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries