Popcorn Lung or Obliterative Bronchiolitis: Diagnostic criteria & treatment by Dr. Jyotsna Joshi
M3 India Newsdesk Oct 16, 2018
Dr. Jyotsna Joshi, a noted Pulmonologist discusses the clinical presentation, diagnostic criteria, and treatment modality for Obliterative Bronchiolitis (OB), also commonly known as Popcorn Lung.

Popcorn disease is synonymous with obronchiolitis obliterans (OB). Obliterative bronchiolitis (OB) or constrictive bronchiolitis (CB) is a specific cause for airway obstruction and is due to the obliteration of respiratory bronchioles or the small airways.
OB contributes significantly to the burden of chronic airway obstruction (CAO) and must be recognised as a distinct clinical entity. CAO is one disorder for which nosology (terminology and classification) is unclear.
Asthma and chronic obstructive pulmonary disease (COPD) are well-recognised causes of CAO. The term asthma and COPD are usually used for diseases with reversible and progressive irreversible airway obstruction respectively. Several disorders remain under-diagnosed due to the uncritical use of these terms. Small airway obstruction may be seen in asthma, COPD and bronchiectasis but is called OB when it occurs alone.
Obliterative bronchiolitis (OB) or constrictive bronchiolitis (CB)
Small airways or respiratory bronchioles are airways <2 mm in diameter and were described in 1960s. They have a vast surface area due to a large branching network. However, they contribute very little to airway resistance. When >80%of the small airways are affected, respiratory symptoms or lung function abnormality develops.
In 2004, CDC reported several cases of bronchiolitis obliterans in workers of a microwave popcorn factory in Missouri. A flavouring agent diacetyl was used to add a buttery flavour to the popcorn. This finding led OB to be named as a “Popcorn Disease”. Although the popcorn manufacturers discontinued the use of diacetyl for their products, people are still being exposed to it through flavoured e-cigarettes.
Common causes leading to popcorn disease
- Chemical exposure in which patients develop disease typically within 2 to 8 weeks
- Transplant surgery may cause some patients to develop popcorn lung
- Exposure to certain drugs such as penicillamine, 5-fluorouracil
- Post-infectious, secondary to childhood viral, mycoplasma infections and post-tuberculosis, commonly seen in developing countries
- Idiopathic causes
Patients who survive the initial bout typically remain stable for several years or progress to end-stage airflow disease and cor pulmonale.
Diagnostic criteria for OB
- Turton et al in 1981 suggested diagnostic criteria for OB as:
- Irreversible airflow obstruction
- Reduced FEV1
- Exclusion of asthma, COPD or other causes of airway obstruction
- Spirometry results
- Classical presentation: Spirometry in OB may show classical obstructive abnormality with or without good bronchodilator reversibility
- Advanced presentation: In advanced disease spirometry may show a greater reduction in FVC than the FEV1, resulting in a normal FEV1 / FVC ratio (false normalisation)
Occasionally there is a paradoxical fall in the FEV1 / FVC ratio following therapy, due to a preferential opening of the small airways causing greater improvement in FVC relative to FEV1.
- High-resolution computed tomography (HRCT)
HRCT in OB shows heterogeneity of lung density i.e. patchy areas of high and low attenuation of the lung parenchyma ("mosaic pattern/ mosaic perfusion") thought to be a consequence of reflex vasoconstriction in under-ventilated areas of the lung with exaggeration on the expiratory scan and is diagnostic in the correct clinical context.
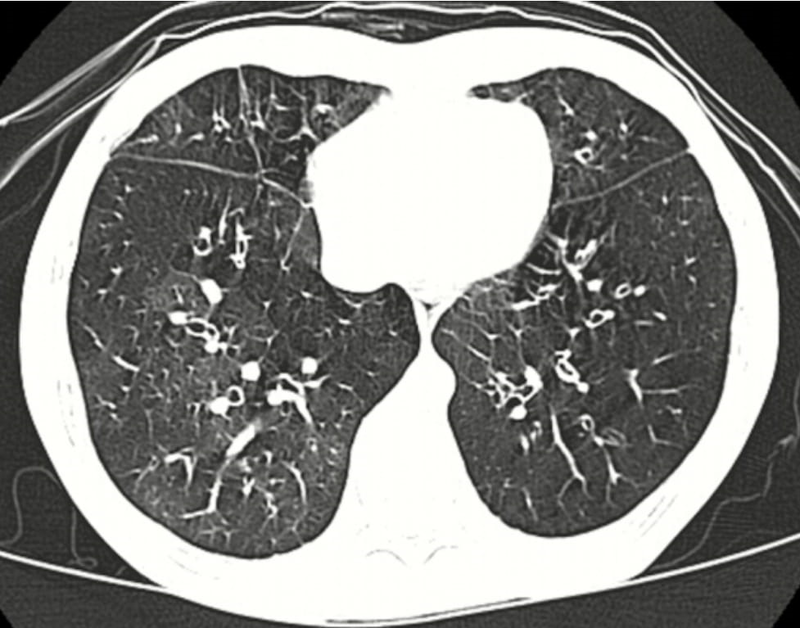 High resolution computed tomography (HRCT) showing mosaic attenuation in a case of OB.
High resolution computed tomography (HRCT) showing mosaic attenuation in a case of OB.
- Open lung biopsy once considered to be the gold standard is not necessary for the diagnosis of OB
Pulmonary Hypertension
Pulmonary HT and cor pulmonale is an important complication of chronic respiratory disorders. The former should, therefore, be suspected in patients with persistent hypoxaemia, who complain of deteriorating exercise tolerance with stable lung functions or in those who develop fluid retention.
Pulmonary hypertension (HT) secondary to chronic respiratory disorders and cor pulmonale are usually caused by chronic hypoxic lung disease including chronic airflow obstruction, fibrosing lung disease and ventilatory failure due to primary chest wall dysfunction, thromboembolic pulmonary disease and connective tissue diseases.
OB may be an important cause for pulmonary HT and cor pulmonale, particularly in young adults. OB should be suspected in case of chronic airway disease with airflow limitation, and HRCT with expiratory scans should be included in the diagnostic algorithm of pulmonary HT.
Differentiating OB with bronchiectasis from bronchiectasis
It is sometimes difficult to make a distinction between post infectious OB which is associated with areas of bronchiectasis, and bronchiectasis with mosaic pattern due to the associated small airway disease.
Hansell et al, found that such changes are common in bronchiectasis and the authors suggested that in these cases, OB might have been an early event in the pathogenesis.
However, bronchiectasis though less frequently seen in the developed world due to the control of childhood infections, is frequently seen in the less developed countries. In most cases childhood, respiratory infections cause either bronchiectasis or OB, however in some individuals both bronchiectasis and OB may result.
In these i.e. OB alone and bronchiectasis with OB, greater airflow limitation due to small airway obstruction perhaps causes early pulmonary HT and cor pulmonale.
Treatment of OB
- Corticosteroids in acute / subacute cases to decrease inflammation
- Immunosuppressive drugs to reduce the activity of the immune system
- Bronchodilators useful in chronic cases
- Oxygen supplement, pulmonary rehabilitation and pneumococcal and influenza vaccines are indicated as adjunct therapies
The therapeutic implication of a diagnosis of OB is that inhaled therapy may not be adequate, and drugs delivered by the systemic route are more likely to reach the large surface area of the small airways.
The best way to prevent popcorn lung is to avoid the factors known to cause the condition.
Disclaimer-The information and views set out in this article are those of the author(s) and do not necessarily reflect the official opinion of M3 India. Neither M3 India nor any person acting on their behalf may be held responsible for the use which may be made of the information contained therein.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries