Primary vs splenic follicular lymphoma: A look inside
M3 Global Newsdesk Jul 02, 2018
A study of the clinical and pathological features of primary splenic follicular lymphoma (FL) shows that it is distinct from systemic FL and it should be managed differently. The results were published in Annals of Hematology.
The study, was led by Joji Shimono, MD, School of Medicine at Kurume University, Japan and the results were published in Annals of Hematology.
The researchers compared the clinicopathological attributes of primary splenic FL and nodal FL. Tissue samples from 17 patients with splenic FL were analyzed and compared with samples from 153 control patients with nodal FL. The only exclusion criterion was a diagnosis of a subtype of FL.
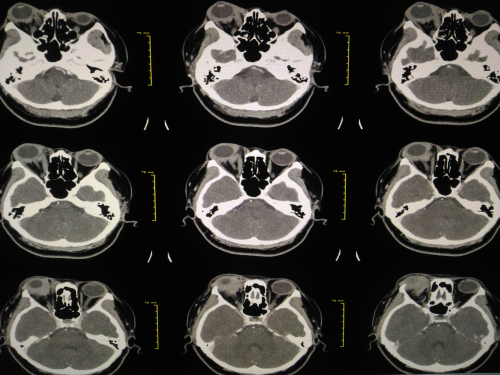
Primary splenic FL is rare, and its clinical and pathological characteristics have not been established. All patients with primary splenic FL underwent splenectomy. In addition, all cases were reviewed by hematopathologists, diagnosed according to the World Health Organization classification (WHO), and had CT imaging.
In the control patients, nodal FL with splenic infiltration was defined as the presence of general lymphadenopathy (enlargement of a lymph node to at least 1.5 cm) and splenic lesions. Cases of splenic lymphoma were identified to not show lymphadenopathy on CT.
- Splenic lymphoma with splenic lesions without general lymphadenopathy was defined as type A.
- Cases with the presence of liver, peripheral blood, or bone marrow infiltration in addition to splenic lesions without general lymphadenopathy were defined as type B.
Second- or third-generation immunoassay kits were used to test for hepatitis C virus (HCV) status. A splenic lesion was considered present if nodular lesions > 3 cm in size were present on CT. Splenomegaly was defined as enlargement of the spleen to a major diameter of ≥ 12 cm on CT.
Flow cytometry, immunohistochemical analysis, fluorescence in situ hybridization analysis, DNA extraction, polymerase chain reaction analysis, and Sanger sequencing of NOTCH1 and NOTCH2 were used to evaluate immunohistochemical and cytogenetic features. Overall survival (OS) was defined as the time of all-cause death. Progression-free survival (PFS) was defined as the time of relapse of FL.
Results showed that 12 of the patients (70.6%) had type A and five (29.4%) had type B splenic FL; four patients (23.5%) were positive for HCV antibodies.
In general, the immunohistochemical and cytogenetic features of splenic FL did not differ from those of nodal FL. The rate of HCV antibody positivity was significantly higher in patients with splenic FL than in those with nodal FL (P=0.02).
The rates of high-risk disease according to the Follicular Lymphoma International Prognostic Index (FLIPI), stage III or IV disease, and MUM1 positivity were all lower in patients with splenic FL than in those with nodal FL (P=0.03, P=0.0003, and P=0.04, respectively).
The investigators noted that there were several differences in clinical features between patients with splenic FL and nodal FL with splenic infiltration. The rate of HCV antibody positivity was higher in patients with splenic FL than in nodal FL with splenic infiltration (P=0.03), leading the team to speculate that HCV infection might be associated with the pathogenesis of splenic lymphoma.
In addition, splenic macronodular lesion positivity was higher in patients with splenic FL than in those with nodal FL with splenic infiltration (P=0.0005).
Furthermore, cases of high risk based on the FLIPI, stage III or IV disease, decreased hemoglobin levels, and histological grades 3A or 3B were more often encountered in patients with splenic FL than in those with nodal FL with splenic infiltration (P=0.04, P=0.0006, P=0.04, and P=0.04, respectively).
The OS and PFS did not significantly differ between patients with splenic FL and nodal FL. The rate of progression was significantly lower in six patients with splenic FL who received chemotherapy compared to 11 who did not receive chemotherapy (P=0.03).
“Splenic FL showed different clinicopathological characteristics from nodal FL,” concluded the authors. “These results suggest that, in such cases, the spleen itself, as the primary lesion, might affect the biological characteristics of FL.” In addition, they noted that splenic FL should be considered a distinct type of FL and should be managed differently than nodal FL.
To read more about this study, click here.
This story is contributed by Robyn Boyle and is a part of our Global Content Initiative, where we feature selected stories from our Global network which we believe would be most useful and informative to our doctor members.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries