Why don’t some people with T1DM react to hypoglycemia? Brain scans give the answer
M3 Global Newsdesk Mar 26, 2018
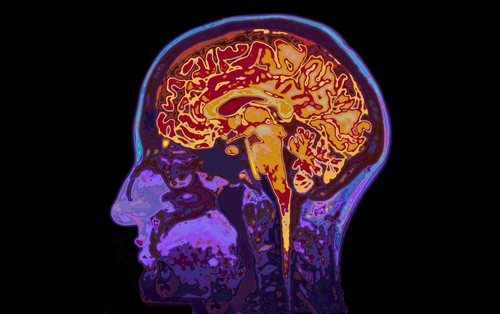
This study, in which researchers used functional magnetic resonance imaging (fMRI) to analyze brain activity, sheds light on why type 1 diabetics with hypoglycemia unawareness don’t respond appropriately by eating and then face dangerous drops in blood glucose levels.
Why are some people with type 1 diabetes mellitus (T1DM) unable to recognize and respond appropriately when their blood glucose level falls? Because of the condition known as hypoglycemia unawareness where their brains, in response to hypoglycemia, become progressively blunted and fail to provoke hunger and other typical reactions, according to researchers who recently published their findings in The Journal of Clinical Investigation.
This study, in which researchers used functional magnetic resonance imaging (fMRI) to analyze brain activity, sheds light on why type 1 diabetics with hypoglycemia unawareness don’t respond appropriately by eating and then face dangerous drops in blood glucose levels.
“Frequent episodes of hypoglycemia in T1DM individuals commonly lead to hypoglycemia-associated autonomic failure, whereby significantly lower blood glucose levels are required to elicit a counterregulatory hormonal response as well as symptomatic awareness of hypoglycemia,” wrote researchers led by Janice Jin Hwang, MD, assistant professor, Division of Endocrinology, Yale School of Medicine, New Haven, CT.
“Whether the loss of hypoglycemia awareness is also accompanied by a failure to activate the drive to eat, which is clinically the most effective way to reverse hypoglycemia, remains unknown,” they added.
Effect on the brain
For this study, Dr. Hwang and colleagues recruited 42 adults: 13 healthy nondiabetics, 16 individuals with T1DM and hypoglycemia awareness, and 13 with T1DM and hypoglycemia unawareness.
The researchers gave all participants insulin to moderately lower their blood glucose levels and then conducted fMRI scans to observe the effects of hypoglycemia on brain activity. The brain scans showed that the three groups had dramatically different responses to lower blood glucose levels, even after adjusting for age and body mass index.
In participants without diabetes, mild hypoglycemia resulted in altered activity in the caudate, insula, prefrontal cortex, and angular gyrus—regions of the brain linked to reward, motivation, and executive control.However, T1DM participants with hypoglycemia awareness showed no changes in the caudate and insula, although they had altered activation patterns in the prefrontal cortex and angular gyrus.“Most strikingly, in direct contrast to healthy controls and T1DM-aware subjects, T1DM-unaware subjects failed to show any hypoglycemia-induced changes in brain activity,” Dr. Hwang and coauthors wrote.
New awareness of unawareness
In addition, both control subjects and T1DM-aware subjects reported significant increases in symptoms during hypoglycemia, yet T1DM-unaware subjects showed no changes in hypoglycemic symptoms.
“Hypoglycemia unawareness in T1DM patients is associated with a diminished brain response to mild hypoglycemia (plasma glucose ~60 mg/dl),” the authors concluded. “Moreover, the pattern of loss of brain responses appears to involve cortico-striatal and fronto-parietal neurocircuits that are known to play important roles in regulating motivation and goal-directed behavior, as well as attention.”
Dr. Hwang further explained, “There is a progressive loss of coordinated brain response to low blood sugar as you go from healthy adult to aware [diabetic] and unaware [diabetic]. The first areas in the brain to go are associated with regulating feeding behavior.”
These findings may help researchers determine how to restore hypoglycemia awareness in patients who have lost it, Dr. Hwang predicted. New technologies for monitoring blood glucose levels could play a part in that effort, she added.
This study was supported in part by grants from the National Institutes of Health and the Yale Center for Clinical Investigation through the Clinical Translational Science Award. Dr. Hwang and corresponding author Robert Sherwin, MD, received research support from Regeneron for work unrelated to this project.
This story is contributed by John Murphy and is a part of our Global Content Initiative, where we feature selected stories from our Global network which we believe would be most useful and informative to our doctor members.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries