2023 ESC Guidelines for the Management of Cardiovascular Disease in Patients with Diabetes
M3 India Newsdesk Sep 20, 2023
This article explains the 2023 ESC guidelines for managing cardiovascular disease in patients with type 2 diabetes, emphasising personalised care, lifestyle changes, and prioritising glucose-lowering medications with proven cardiovascular benefits.
Diabetic patients are at increased risk of cardiovascular diseases. CVD manifests as Coronary artery disease (CAD), heart failure (HF), stroke, Atrial fibrillation (AF), aortic disease and peripheral artery disease (PAD).
The latest guidelines for 2023 from the European Society of Cardiology (ESC) on the management of CVD in diabetic patients are designed to help treating clinicians prevent and manage the manifestation of CVD in patients with diabetes.
The last decade has been exciting in terms of new molecules such as sodium–glucose co-transporter-2 (SGLT2) inhibitors and glucagon-like peptide-1 (GLP-1) receptor agonists (RAs), non-steroidal mineralocorticoid receptor antagonists (MRAs), such as finer enone which has substantially expanded available therapeutic options for such patient-population.
The various CVOTs (Cardiovascular Outcome Trials) over the years have resulted in numerous evidence-based recommendations for the management of diabetic patients with CVD.
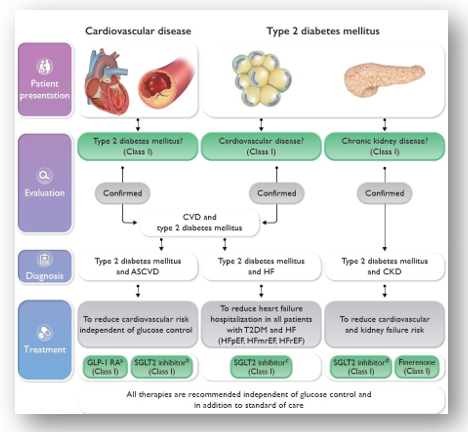
Management of cardiovascular disease in patients with type 2 diabetes
Recommendations for diagnosis of diabetes
Screening for diabetes is recommended in all individuals with CVD, using fasting glucose and/or HbA1c or on an OGTT if still in doubt.
Recommendations for assessing cardiovascular risk in patients with diabetes
- It is recommended that patients with diabetes be screened for the presence of severe target organ damage (TOD).
- It is recommended to assess medical history and the presence of symptoms suggestive of ASCVD in patients with diabetes.
- In patients with T2DM without symptomatic ASCVD or severe TOD, it is recommended to estimate 10-year CVD risk via SCORE2-Diabetes.
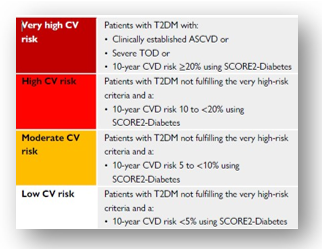
Cardiovascular risk categories in type 2 diabetes
Recommendations for general measures like weight reduction, nutrition, physical activity/exercise, and smoking cessation in patients with diabetes
- It is recommended that individuals living with overweight or obesity aim to reduce weight and increase physical exercise to improve metabolic control and overall CVD risk profile.
- It is recommended to adopt a Mediterranean or plant-based diet with high unsaturated fat content to lower cardiovascular risk.
- It is recommended to increase any physical activity in all patients with T2DM with and without CVD. Optimal is a weekly activity of 150 min of moderate intensity or 75 min of vigorous endurance intensity.
- It is recommended to introduce structured exercise training in patients with T2DM and established CVD, to improve metabolic control, exercise capacity and quality of life, and to reduce CV events.
- It is recommended to stop smoking to reduce cardiovascular risk.
Recommendations for glycaemic targets
- It is recommended to apply tight glycaemic control (HbA1c <7%) to reduce microvascular complications.
- It is recommended to avoid hypoglycaemia, particularly in patients with CVD.
- It is recommended to individualise HbA1c targets according to co-morbidities, diabetes duration, and life expectancy.
Recommendations for glucose-lowering treatment for patients with type 2 diabetes and atherosclerotic cardiovascular disease to reduce cardiovascular risk
It is recommended to prioritise the use of glucose-lowering agents with proven CV benefits followed by agents with proven CV safety over agents without proven CV benefits or proven CV safety.
1. Sodium-glucose co-transporter-2 inhibitors
SGLT2 inhibitors with proven CV benefit are recommended in patients with T2DM and ASCVD to reduce CV events, independent of baseline or target HbA1c and independent of concomitant glucose-lowering medication.
2. Glucagon-like peptide-1 receptor agonists
GLP-1 RAs with proven CV benefit are recommended in patients with T2DM and ASCVD to reduce CV events, independent of baseline or target HbA1c and independent of concomitant glucose-lowering medication.
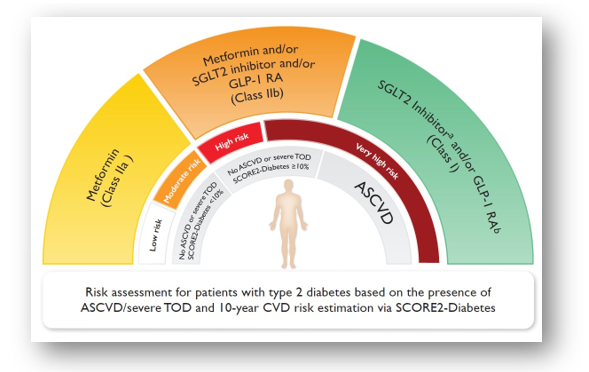
Glucose-lowering treatment for patients with type 2 DM to reduce CV risk based on the presence of ASCVD/severe target-organ damage
Recommendations for blood pressure in patients with diabetes
1. Screening for hypertension
Regular BP measurements are recommended in all patients with diabetes to detect and treat hypertension to reduce CV risk.
2. Treatment targets
- Anti-hypertensive drug treatment is recommended for people with diabetes when office BP is ≥140/90 mmHg.
- It is recommended to treat hypertension in patients with diabetes in an individualised manner. The BP goal is to target SBP to 130 mmHg and <130 mmHg if tolerated, but not <120 mmHg. In older people (age >65 years), it is recommended to target SBP to 130–139 mmHg.
- Lifestyle changes (weight loss if overweight, physical activity, alcohol restriction, sodium restriction, increased consumption of vegetables, using low-fat dairy products) are recommended in patients with diabetes and hypertension.
- It is recommended to initiate treatment with a combination of an RAS inhibitor and a CCB or thiazide/thiazide-like diuretic. Guidelines do not recommend the combination of ACE inhibitors and ARB.
Recommendation for lipid targets in patients with diabetes
- In patients with T2DM at moderate CV risk, an LDL-C target of <2.6 mmol/L (<100 mg/dL) is recommended.
- In patients with T2DM at high CV risk, an LDL-C target of <1.8 mmol/L (<70 mg/dL) and LDL-C reduction of at least 50% is recommended.
- In patients with T2DM at very high CV risk, an LDL-C target of <1.4 mmol/L (<55 mg/dL) and LDL-C reduction of at least 50% is recommended.
- In patients with T2DM, a secondary goal of a non-HDL-C target of <2.2 mmol/L (<85 mg/dL) in very high CV risk patients, and <2.6 mmol/ L (<100 mg/dL) in high CV risk patients, is recommended.
Lipid-lowering treatment in patients with diabetes
- Statins are recommended as the first-choice LDL-C-lowering treatment in patients with diabetes and above-target LDL-C levels. Administration of statins is defined based on the CV risk profile of the patients and the recommended LDL-C (or non-HDL-C) target levels.
- If the target LDL-C is not reached with statins, combination therapy with ezetimibe is recommended.
- A PCSK9 inhibitor is recommended in patients at very high CV risk, with persistently high LDL-C levels above target despite treatment with a maximum tolerated statin dose, in combination with ezetimibe, or in patients with statin intolerance.
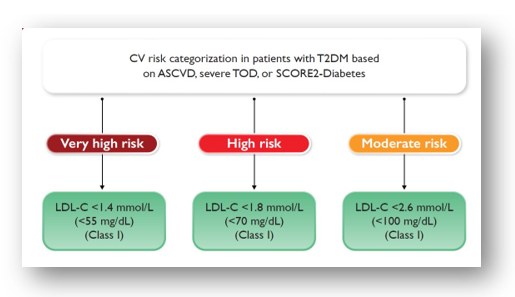
Recommended LDL-cholesterol targets by cardiovascular risk categories in patients with type 2 diabetes
Recommendations for antithrombotic therapy in patients with diabetes and acute or chronic coronary syndrome without indications for long-term oral anticoagulation
- Aspirin at a dose of 75–100 mg o.d. is recommended in patients with diabetes and previous MI or revascularisation (CABG or stenting).
- In patients with ACS and diabetes who undergo PCI, a P2Y12 receptor inhibitor (ticagrelor or prasugrel) is recommended in addition to ASA (75–100 mg o.d.), maintained over 12 months.
- Clopidogrel 75 mg o.d. following appropriate loading (e.g. 600 mg or at least 5 days already on maintenance therapy) is recommended in addition to ASA for 6 months following coronary stenting in patients with CCS, irrespective of stent type, unless a shorter duration is indicated due to the risk or occurrence of life-threatening bleeding.
- Clopidogrel is recommended as an alternative in case of ASA intolerance.
- In patients with diabetes and ACS treated with dual antiplatelet therapy (DAPT) who are undergoing CABG and do not require long-term OAC therapy, resuming a P2Y12 receptor inhibitor as soon as deemed safe after surgery and continuing it up to 12 months is recommended.
Recommendations for antithrombotic therapy in patients with diabetes and acute or chronic coronary syndrome and/or post-percutaneous coronary intervention requiring long-term oral anticoagulation
- In patients with Atrial fibrillation and receiving anti-platelet therapy, eligible for anticoagulation, and without a contraindication, NOACs are recommended in preference to a Vitamin K antagonist.
- In patients with ACS or CCS and diabetes undergoing coronary stent implantation and having an indication for anticoagulation, triple therapy with low-dose ASA, clopidogrel, and an OAC is recommended for at least 1 week, followed by dual therapy with an OAC and a single, oral, anti-platelet agent.
Recommendations for gastric protection
- When antithrombotic drugs are used in combination, proton pump inhibitors are recommended to prevent gastrointestinal bleeding.
- When clopidogrel is used, omeprazole and esomeprazole are not recommended for gastric protection.
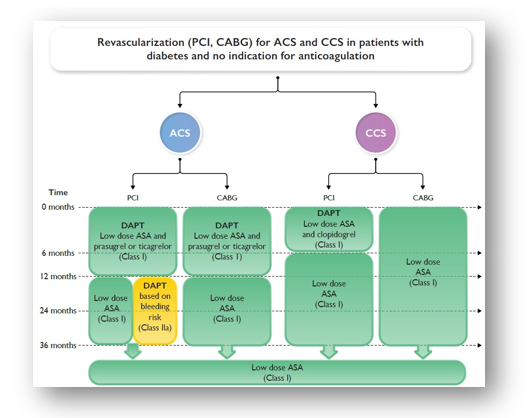
Recommendations for antiplatelet therapy in patients with diabetes with Acute or chronic coronary syndrome
Recommendations for heart failure screening and diagnosis in patients with diabetes
Evaluation for heart failure
If HF is suspected, it is recommended to measure BNP/NT-proBNP. A systematic survey for HF symptoms and/or signs of HF is recommended at each clinical encounter in all patients with diabetes.
Recommendations for heart failure treatments in patients with heart failure with reduced ejection fraction and diabetes
Recommendations for pharmacological treatment indicated in patients with HFrEF (NYHA class II-IV) and diabetes
- SGLT2 inhibitors (dapagliflozin, empagliflozin, or sotagliflozin) are recommended in all patients with HFrEF and T2DM to reduce the risk of HF hospitalisation and death.
- Sacubitril/valsartan or an ACE-I is recommended in all patients with HFrEF and diabetes to reduce the risk of HF hospitalisation and death.
- Beta-blockers are recommended in patients with HFrEF and diabetes to reduce the risk of HF hospitalisation and death.
- MRAs are recommended in patients with HFrEF and diabetes to reduce the risk of HF hospitalisation and death.
- An intensive strategy of early initiation of evidence-based treatment (SGLT2 inhibitors, ARNI/ACE-Is, beta-blockers, and MRAs), with rapid up-titration to trial-defined target doses starting before discharge and with frequent follow-up visits in the first 6 weeks following an HF hospitalisation is recommended to reduce re-admissions or mortality.
- ARBs are recommended in symptomatic patients with HFrEF and diabetes who do not tolerate sacubitril/valsartan or ACE-Is, to reduce the risk of HF hospitalisation and death.
- Diuretics are recommended in patients with HFrEF and diabetes with signs and/or symptoms of fluid congestion to improve symptoms, exercise capacity, and HF hospitalisation.
Recommendations for the treatment of heart failure patients with left ventricular ejection fraction >40% and diabetes
- Empagliflozin or dapagliflozin are recommended in patients with T2DM and LVEF >40% (HFmrEF and HFpEF) to reduce the risk of HF hospitalisation or CV death.
- Diuretics are recommended in patients with HFpEF or HFmrEF and diabetes with signs and/or symptoms of fluid congestion to improve symptoms, exercise capacity, and HF hospitalisation.
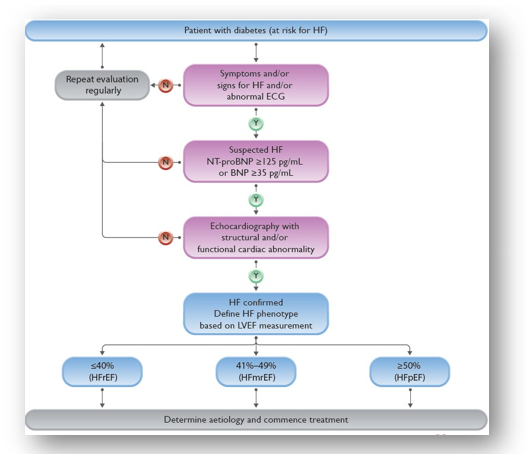
Diagnostic algorithm for heart failure in patients with diabetes
Recommendations for glucose-lowering medications to reduce heart failure hospitalisation in patients with type 2 diabetes with or without existing heart failure
- SGLT2 inhibitors (empagliflozin, canagliflozin, dapagliflozin, ertugliflozin, or sotagliflozin) are recommended in patients with T2DM with multiple ASCVD risk factors or established ASCVD to reduce the risk of HF hospitalisation.
- SGLT2 inhibitors (dapagliflozin, empagliflozin, or sotagliflozin) are recommended in patients with T2DM and HFrEF to reduce the risk of HF hospitalisation and death.
- Empagliflozin or dapagliflozin are recommended in patients with T2DM and LVEF >40% (HFmrEF and HFpEF) to reduce the risk of HF hospitalisation or CV death.
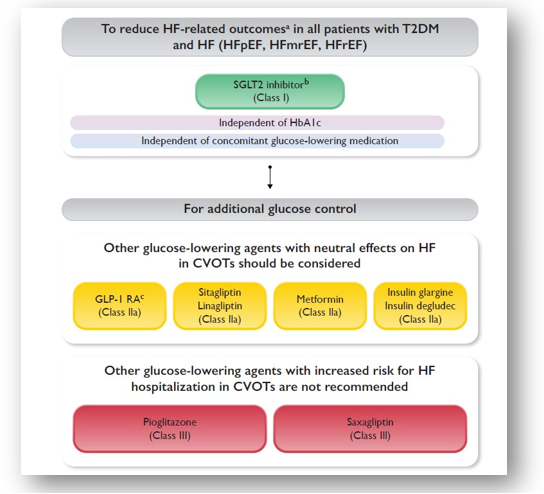
Glucose-lowering treatment of patients with heart failure and type 2 diabetes
Recommendations for glucose-lowering medications with an increased risk of heart failure hospitalisation in patients with type 2 diabetes
- Pioglitazone is associated with an increased risk of incident HF in patients with diabetes and is not recommended for glucose-lowering treatment in patients at risk of HF (or with previous HF).
- The DPP-4 inhibitor saxagliptin is associated with an increased risk of HF hospitalisation in patients with diabetes and is not recommended for glucose-lowering treatment in patients at risk of HF (or with previous HF).
Recommendations for atrial fibrillation screening in patients with diabetes, and anticoagulation for atrial fibrillation in patients with diabetes
- Opportunistic screening for AF by pulse taking or ECG is recommended in patients ≥65 years of age.
- Opportunistic screening for AF by pulse taking or ECG is recommended in patients with diabetes <65 years of age (particularly when other risk factors are present) because patients with diabetes exhibit a higher AF frequency at a younger age.
- Oral anticoagulation is recommended for preventing stroke in patients with AF and diabetes and with at least one additional (CHA2DS2-VASc) risk factor for stroke.
- For preventing stroke in AF, NOACs are recommended in preference to VKAs, with the exception of patients with mechanical valve prostheses or moderate to severe mitral stenosis.
Recommendations for patients with chronic kidney disease and diabetes
- Intensive LDL-C lowering with statins or a statin/ezetimibe combination is recommended in dyslipidemia.
- A blood pressure target of ≤130/80 mmHg is recommended to reduce the risk of CVD and albuminuria.
- Personalised HbA1c targets 6.5–8.0% (48–64 mmol/mol) are recommended, with a target <7.0% (<53 mmol/mol) to reduce microvascular complications, wherever possible.
- The maximum tolerated dose of an ACE-I or ARB is recommended. Combined use of an ARB with an ACE-I is not recommended.
- An SGLT2 inhibitor (canagliflozin, empagliflozin, or dapagliflozin) is recommended in patients with T2DM and CKD with an eGFR ≥20 mL/min/1.73 m2 to reduce the risk of CVD and kidney failure.
- Finerenone is recommended in addition to an ACE-I or ARB in patients with T2DM and eGFR >60 mL/min/1.73 m2 with a UACR ≥30 mg/mmol (≥300 mg/g), or eGFR 25–60 mL/min/1.73 m2 and UACR ≥3 mg/mmol (≥30 mg/g) to reduce CV events and kidney failure.
- A GLP-1 RA is recommended at eGFR >15 mL/min/1.73 m2 to achieve adequate glycaemic control, due to low risk of hypoglycaemia and beneficial effects on weight, CV risk, and albuminuria.
- Low-dose ASA (75–100 mg o.d.) is recommended in patients with CKD and ASCVD.
- It is recommended that patients with diabetes are routinely screened for kidney disease by assessing eGFR defined by CKD-EPI and UACR.
- Treatment with intensive medical or an initial invasive strategy is recommended in people with CKD, diabetes, and stable moderate or severe CAD, due to similar outcomes.
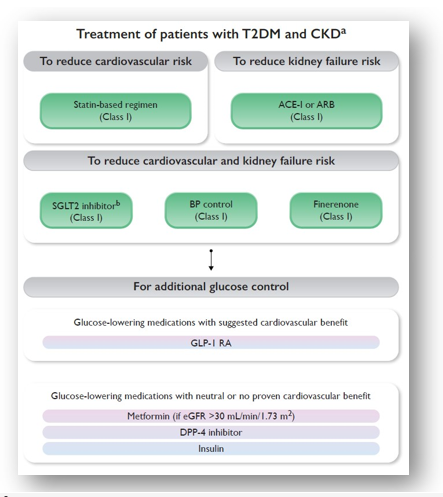
Treatment to reduce CV or kidney failure risk in patients with type 2 diabetes and CKD
Recommendations for aortic and peripheral arterial diseases and diabetes
Lower-extremity artery disease in patients with diabetes
- In patients with diabetes and symptomatic LEAD, antiplatelet therapy is recommended.
- In patients with diabetes and Chronic limb-threatening ischemia (CLTi), it is recommended to assess the risk of amputation; the WIfI score is useful for this purpose.
- As patients with diabetes and LEAD are at very high CV risk, an LDL-C target of <1.4 mmol/L (<55 mg/dL) and an LDL-C reduction of at least 50% is recommended.
- Screening for LEAD is recommended on a regular basis, with clinical assessment and/or ABI measurement.
- Patient education about foot care is recommended in patients with diabetes, especially those with LEAD, even if asymptomatic. Early recognition of tissue loss and/or infection, and referral to a multidisciplinary team, are mandatory to improve limb salvage.
- An Ankle-brachial index of ≤0.90 is diagnostic of LEAD, irrespective of symptoms. In symptomatic cases, further assessment including duplex ultrasound is recommended.
- When ABI is elevated (>1.40), other non-invasive tests, including TBI or duplex ultrasound, are recommended.
- Duplex ultrasound is recommended as the first-line imaging method to assess the anatomy and haemodynamic status of lower-extremity arteries.
- In the case of CLTI, revascularisation is recommended whenever feasible for limb salvage.
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr Hitesh Saraogi is a diabetologist, physician and an obesity specialist at Dhanvantari Hospital, Raj Nagar Extension, Ghaziabad.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries