Post-COVID cardiovascular sequelae: Latest MoHFW updates
M3 India Newsdesk Feb 24, 2022
Post testing positive for COVID-19, many people have been reported to be suffering from short to long-term effects of the illness. Cardiovascular sequelae can be observed in not only symptomatic COVID-19 patients but have also been reported in asymptomatic patients. Physicians should be aware of these symptoms and the cardiovascular implications of COVID-19.
As the pandemic enters its third year, people who have persistent symptoms after recovering from COVID-19 are becoming more widely recognised as a rising group in need of care. Many people have been reported to be suffering from short to long-term effects of the illness. Some people continue to have side effects or symptoms that may or may not be related to COVID-19.
Key takeaways
- Up to 20% to 30% of patients hospitalised with severe COVID-19 have evidence of myocardial involvement manifested by elevated troponin levels, venous thromboembolism, heart failure and arrhythmias.
- Chest pain, dyspnea and palpitations are well-described symptoms in patients with cardiac sequelae.
- Post-COVID patients with persistent cardiac symptoms should undergo chest radiograph, ECG, echocardiography and cardiac biomarkers (Troponins/NT-pro-BNP) to assess cardiovascular involvement.
- Evidence-based treatment of cardiovascular Long COVID is mandated to reduce the long term impact of COVID-19.
Acute COVID vs Long COVID
In the lack of a globally agreed terminology, the Post-COVID syndrome is described as signs and symptoms that appear during or after an infection that is consistent with COVID-19 and last for more than 12 weeks and cannot be explained by any other diagnosis.
In recent research, Post-COVID patients have been divided into two categories:
- Subacute or continuing symptomatic COVID (4-12 weeks after acute COVID-19)
- Chronic COVID or Post-COVID syndrome (symptoms lasting beyond 12 weeks after acute COVID-19)
Another popular term is "Long COVID," which is described by the National Institute for Health and Care Excellence as symptoms that persist or worsen after acute COVID-19.
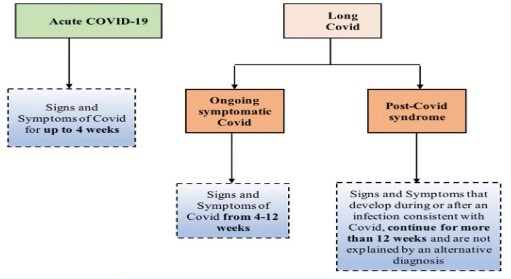
Terminology and definition of Long COVID
Guideline updates on the Post-COVID cardiovascular sequel
- Cardiovascular complications have been described in both symptomatic and asymptomatic COVID-19 individuals.
- Up to 20% to 30% of patients hospitalised with severe COVID-19 exhibit signs of cardiac involvement, as seen by raised troponin levels, venous thromboembolism, heart failure, and arrhythmias. Troponin elevations have been related to poor outcomes and greater in-hospital death rates in acute symptomatic patients.
- Numerous hypotheses have been advanced to account for the cardiovascular problems associated with COVID-19.
- Cardiomyocytes have been damaged directly or as a result of hypoxia, microvascular dysfunction, thrombosis, and cytokine storm.
- Given the high incidence of cardiac damage, a spectrum of heart disease is conceivable, with some lingering post myocarditis abnormalities in severe instances.
- Myocardial involvement is thought to be the starter of the inflammatory process and subsequent fibrosis (seen on cardiac magnetic resonance imaging) as well as long-term consequences. Long-term complications include increased cardiometabolic demand, myocardial fibrosis or scarring, chronic left ventricular dysfunction, heart failure, arrhythmias, inappropriate sinus tachycardia, and autonomic dysfunction.
- Many of the persistent signs and symptoms are seen in patients after COVID-19 recovery including tiredness, dyspnea, and chest discomfort - are non-specific. This may develop spontaneously in asymptomatic COVID-19 individuals or in symptomatic COVID-19 patients who do not have clinically obvious cardiac involvement during the acute phase.
- During the acute phase, patients who acquire viral myocarditis, myocardial infarction, pulmonary embolism, stress-induced myocardial damage, and arrhythmias are at increased risk of developing long-term cardiovascular problems and poor outcomes. These subgroups of patients often have comorbidities that hamper their post-acute phase recovery. They include:
- Diabetes
- Hypertension
- Obesity
- Dyslipidemia
- Chronic renal disease
At sixty-day follow-up, 20% of COVID-19 survivors reported experiencing chest discomfort. Palpitations have been documented in 10% of COVID-19 survivors after sixty days. At six months post-acute COVID-19, ongoing chest discomfort and palpitations were recorded in 5% and 9% of patients, respectively. When compared to pre-pandemic periods, stress cardiomyopathy is 4-5 times more prevalent during the COVID-19 pandemic (7.8 per cent versus 1.5-1.8 per cent).
In one research, myocardial inflammation revealed on cardiac MRI was discovered in up to 60% of afflicted individuals more than two months following diagnosis. However, this high rate of cardiac involvement has not been confirmed in other research, and the clinical consequences of these results, if any, are unknown.
In post-acute COVID-19 patients, retrospective investigations have shown a 5% risk of venous thromboembolism. However, the great majority of people with asymptomatic/mild COVID-19 do not have any severe complications. Comparing survivors of COVID-19 infection to controls, case-control studies revealed no evidence of increased cardiac involvement.
Clinical characteristics: Manifestations of symptoms
In most persons with long COVID, the most frequent symptom is severe tiredness. Other symptoms such as chest discomfort, dyspnea, and palpitations are well-documented in individuals with cardiac complications. On the basis of location, aggravating and relieving variables, chest pain consistent with classic angina should be distinguished from atypical or non-anginal chest pain. Similarly, respiratory and cardiac causes of dyspnea must be distinguished.
A high index of suspicion for cardiac dyspnea, particularly in the context of acute coronary syndrome, pulmonary embolism, myocarditis, and tachyarrhythmias, is critical for detecting deteriorating cardiac state and beginning appropriate therapy early. Palpitations may occur as a result of inappropriate sinus tachycardia, postural orthostatic tachycardia syndrome caused by a hyperadrenergic condition or premature ventricular contractions, or ventricular arrhythmias caused by myocardial fibrosis and scarring.
Syncope of neurological origin must be distinguished from that of cardiogenic origin using a thorough history, attentive examination, and applicable tests such as an electrocardiogram (ECG) and a Holter monitor. Patients with heart illness (pre-COVID or during acute infection) should be suspected of heart failure who have:
- Tachycardia
- Neck vein distention
- Dyspnea
- Orthopnea
- Paroxysmal nocturnal dyspnea
- Pedal oedema
- Hepatomegaly
- Left ventricular third heart sound
Investigations
After follow-up, patients who have cardiovascular problems during an acute infection or who have persistent heart symptoms may undergo serial clinical, ECG, and echocardiography examinations. The figure below illustrates a strategy for identifying individuals with cardiac damage during the acute and convalescent phases.
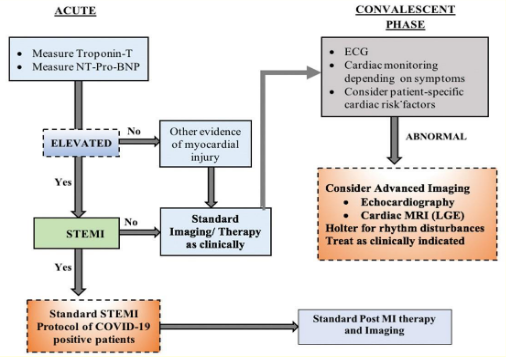
Recommendations to identify patients with a cardiac injury during acute and convalescent-phase
Patients assessed at Post-COVID clinics with persistent cardiac symptoms should have a chest radiograph, electrocardiogram, and cardiac biomarkers (Troponins/NT-pro-BNP) to rule out cardiovascular involvement. Additional diagnostic procedures may be suggested based on symptoms and screening investigations such as:
- Echocardiography
- Cardiac magnetic resonance imaging (MRI)
- Cardiopulmonary exercise testing
- Holter rhythm monitoring
- Chest CT
- Lower extremity Doppler testing
Management of Post-COVID cardiovascular sequelae
The care of patients with Post-COVID cardiovascular sequelae is determined by their pre-existing cardiac comorbidities and the cardiac condition that emerged during the acute phase (myocardial infarction, pulmonary embolism, tachyarrhythmias, etc.) or after recovery. The following table summarises common dos and don'ts during the Post-COVID phase.
Common do's and don'ts during Post COVID period
- Frequent hand washing and social distancing should be followed.
- Restructure routines at home.
- Greater emphasis on a healthy weight and healthy eating habits.
- Moderate intensity exercise (30 minutes per day to 5 times a week).
- Avoid alcohol, smoking or tobacco products.
- Self-medication, or over the counter medication should be avoided.
- Arrange telemedicine contacts for follow up.
- Vaccination after 3 months post-recovery if not vaccinated prior.
- Important to control HT, DM and dyslipidemia. Follow guideline-directed medical therapies for CV risk factors.
- Practice meditation and yoga within tolerance limits.
- Limit activities to 60%of maximum heart rate until 2-3 weeks after symptoms resolve.
- Intense cardiovascular exercise in known cardiac patients and all cardiovascular training in case of athletes to be avoided for 3 months.
- Do not ignore warning signs such as high grade fever, oxygen saturation <93%, chest pain, dizziness, syncope or palpitations.
Impact of cardiovascular activities on Post COVID patients
Cardiopulmonary exercise's effect on Post-COVID patients is unknown at the moment. However, basic guidelines that apply to this subgroup of patients include one week of low-intensity stretching and strengthening before activity in patients with moderate COVID-19 post-recovery.
In the case of moderate Post-COVID symptoms, it is advisable to restrict exertion to slow walking and increase rest time if symptoms intensify. Limit activity to 60% of maximal heart rate (220-age in years) in individuals with persisting symptoms (such as weariness, cough, dyspnea, or fever) for 2-3 weeks after symptoms diminish.
For three months, all patients should abstain from strenuous cardiovascular activity. Athletes are recommended to take three months off cardiovascular exercise and follow up with a specialist, with a reintroduction to sport based on functional status, biomarkers, the absence of dysrhythmias, and evidence of normal left ventricular systolic function.
Patients with cardiac comorbidities/diseases such as diabetes mellitus, hypertension, obesity, atrial fibrillation, and previous myocardial infarction or heart failure should be addressed with utmost care according to guideline-directed medical treatment. Patients with cardiovascular disease should be on statins and antiplatelet medications in addition to medications for risk factor management, such as hypertension and diabetes.
Adequate treatment of cardiac risk factors such as diabetes, hypertension, obesity, and dyslipidemia, in addition to the lifestyle modifications described above, is critical in this ongoing pandemic to avoid not only the development of new cardiac complications but also to avoid decompensation in those who already have heart disease. Serial follows up of these patients biannually or annually is the key to ensuring drug compliance and avoiding further major adverse cardiac events.
Nonpharmacological therapies
- Nonpharmacological therapy options for persons with congestive heart failure include education about self-management, limiting dietary salt to <2g/day and fluid consumption to<2 L/day (1.5 L for severe CHF), explaining dyspnea, oedema, bloating, and smoking cessation.
- They are encouraged to contact their cardiologist immediately or through telemedicine if their symptoms worsen or if they need routine follow-up. Prior data implies that people with cardiovascular disease are at an increased risk of cardiovascular events after severe viral infections.
- As of now, data from the continuing pandemic are limited, and vaccination against COVID-19 and pneumococcal illness is advised. Beta-blockers, Angiotensin-Converting Enzyme Inhibitors (ACE inhibitors)/Angiotensin Receptor-Neprilysin Inhibitors (ARNi)/Angiotensin Receptor Blockers (ARB), mineralocorticoid receptor blockers, and diuretics are all examples of pharmacological treatment for heart failure that is guided by guidelines.
- Anticoagulation is required for stroke prevention in patients with atrial fibrillation, as determined by the CHA2DS2Vasc score. Patients with proven DVT/pulmonary embolism need prophylaxis with anticoagulants, preferably new oral anticoagulants or warfarin, to maintain an INR (international normalised ratio) of 2-3.
COVID-19 has an effect on the cardiovascular system during the recovery period and is considered to be a component of the overall Post-COVID syndrome. Physicians treating Post-COVID clinics should be aware of these symptoms and cardiovascular consequences of COVID-19 sequelae. Cardiovascular disease screening, appropriate investigations, and evidence-based therapy of long COVID is required to mitigate the long-term effects of COVID-19.
The guidelines for post COVID sequel by MoHFW will be discussed in this series pertaining to different organ systems- Cardiovascular, Gastrointestinal, Nephrological, Neurological, and Respiratory. This is the first part of the Post-COVID syndromes series. Stay tuned for the next part.
Disclaimer- The views and opinions expressed in this article are those of the author's and do not necessarily reflect the official policy or position of M3 India.
The author is a practising super specialist from New Delhi.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries