2020 GOLD guidelines for COPD & what they mean for Indian doctors: Dr. Ashok Mahashur
M3 India Newsdesk Jun 25, 2020
Dr. Ashok Mahashur, picks key practice points from the recent 2020 GOLD guidelines on COPD and explains their application in the Indian context.

Chronic Obstructive Pulmonary Disease (COPD) is a common, preventable and treatable disease that is characterised by persistent respiratory symptoms and airflow limitation that is due to airway and/or alveolar abnormalities usually caused by significant exposure to noxious particles or gases and influenced by host factors including abnormal lung development. Significant comorbidities may have an impact on morbidity and mortality.
COPD is the result of a complex interplay of long-term cumulative exposure to noxious gases and particles, combined with a variety of host factors including genetics, airway hyper-responsiveness and poor lung growth during childhood. Worldwide, the most commonly encountered risk factor for COPD is tobacco smoking. On the contrary, in our country, a major cause for COPD is biomass fuel exposure in indoor and outdoor settings. These inciting factors lead to impaired lung growth, accelerated lung damage and inflammation all over.
Diagnosis
Clinical presentation of COPD comprises of an individual mostly aged more than 40 years with persistent progressive dyspnoea, cough with or without expectoration and recurrent respiratory tract infection in presence of risk factors like smoking history or biomass fuel exposure. Such a scenario warrants further evaluation to establish the diagnosis of COPD.
Diagnosis mandatorily requires spirometry assessment to demonstrate objectively, airflow limitation. It is a non-invasive, readily available and affordable test. Despite its good sensitivity, peak expiratory flow measurement alone cannot be reliably used as the only diagnostic test because of its weak specificity. Spirometry is helpful for diagnosis, severity grading and follow up assessment for therapeutic decisions. Presence of a post-bronchodilator FEV1/FVC < 0.70 confirms the presence of persistent airflow limitation and thus of COPD in patients with appropriate symptoms and significant exposures to noxious stimuli.
As per GOLD guidelines, COPD can be graded in four different groups as depicted in table 1 (in patients with FEV1/FVC < 0.7 ). Alpha 1 antitrypsin deficiency should be considered in those few patients who present early in age with localised emphysema and strong family history of similar illness.
Table 1. Classification of airflow limitation severity in COPD (based on postbronchodilator FEV1)
| GOLD 1 | Mild | FEV1 >80 % predicted |
| GOLD 2 | Moderate | FEV1: 50%-80% predicted |
| GOLD 3 | Severe | FEV1: 30%-50% predicted |
| GOLD 4 | Very severe | FEV1 < 30 % predicted |
Other additional tests can be done which help either with overall assessment or act as supportive tools.
- X-ray chest doesn’t help n diagnosis directly but helps to rule out possible differentials
- HRCT scan helps rule out bronchiectasis, as a screening for lung cancer if suspected, and, rules out alternative diagnosis and as a pre-requisite for lung volume reduction surgery
- A 6-minute walk test helps assess functional exercising capacity, diffusion analysis and lung volumes to understand the magnitude of illness
- Pulse oximetry is used to assess all patients with clinical signs suggestive of respiratory failure or right heart failure
- If peripheral arterial oxygen saturation is <92% arterial or capillary blood gases should be assessed
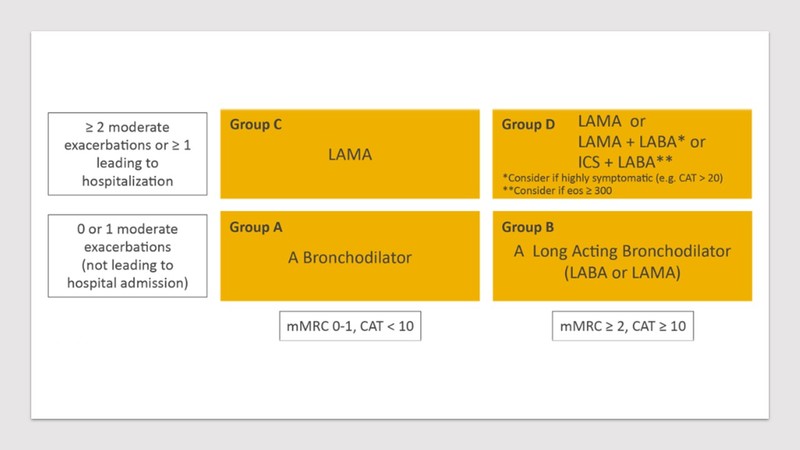
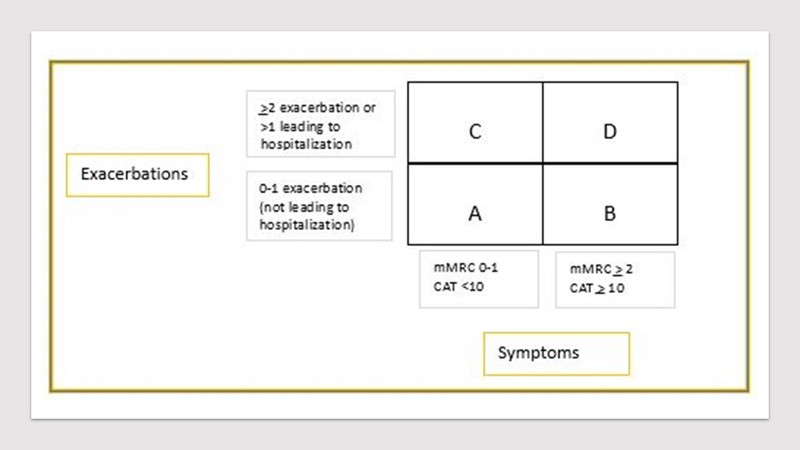
Once confirmed on spirometry analysis, all COPD patients should be analysed for severity of airflow limitation. Thereafter, assessment of symptoms and risk for exacerbation is essential to categorise them into ABCD assessment algorithm. Refined ABCD tool only requires level of symptoms as per modified British Medical Research Council score (mMRC) or COPD Assessment Test (CAT) scores (Figure 1).
Figure 1. ABCD assessment tool for classification of COPD
Treatment of COPD
Aim of therapy is to achieve better symptom control, reduce exacerbation frequency and intensity, enhance quality of life with better effort tolerance and participation in daily living. Comprehensive treatment of COPD involves both pharmacological and non-pharmacological interventions.
Pharmacotherapy in COPD
Pharmacotherapy in COPD primarily consists of bronchodilators and anti-inflammatory agents which are delivered either through inhaled or systemic routes depending upon clinical history. Through inhaled route, bronchodilators (beta 2 agonists and antimuscarinics) and anti-inflammatory (inhaled corticosteroids) are administered. Likewise, through systemic route, glucocorticoids, PDE4 inhibitors, antibiotics, theophylline. Importantly, despite the benefits achieved with all the pharmacological agents, unfortunately no medication has yet achieved reduction in long term decline of lung function.
Table 2. Inhaled bronchodilators in COPD
A. Beta 2 agonists
| Short-acting beta2 agonist (SABA) | Long-acting beta 2 agonist (LABA) |
|
Fenoterol |
Aformoterol |
B. Antimuscarinics
| Short-acting drugs (SAMA) | Long-acting drugs (LAMA) |
|
Ipratropium bromide |
Aclidinium bromide |
After a thorough assessment of clinical details, COPD patients should be classified in ABCD scheme as per their level of symptoms and number of exacerbations. As per the category, treatment should be initiated as described below in Figure 2 (GOLD guidelines). From group A to D severity of illness rises and thus the revision is warranted.
- For a person who falls in Group A (mild or no symptoms with at most single episode of exacerbation not requiring hospitalisation), inhaled bronchodilators should be initiated (short-acting or long-acting agents) and continued if benefits noted.
- Group B (more symptomatic with mMRC>2 and have had at most single episode of exacerbation not requiring hospitalisation), a long-acting inhaled bronchodilator (LABA or LAMA) should be initiated. For those who present with severe breathlessness, combination therapy (LABA and LAMA) should be started upfront. Patients in this group are usually found with comorbidities, which should be managed simultaneously.
- In Group C patients (mildly symptomatic with mMRC < 2 with more risk of exacerbation i.e. >2 moderate exacerbation or >1 requiring hospitalisation), single inhaled bronchodilator should be initiated. In this group LAMA is preferred over LABA due to more risk of exacerbations.
- In Group D (more symptomatic with mMRC>2 and have more risk of exacerbation i.e. >2 moderate exacerbation or >1 requiring hospitalisation), therapy should be started with LAMA monotherapy. However, if the patient is found to be overtly symptomatic, a combination therapy (LABA and LAMA) should be considered. In a subset of patients, where there has been a past or concomitant history of asthma, blood eosinophil counts >300 cells/ul, inhaled corticosteroids should be considered as a combination with LABA. Risk of pneumonia with ICS should always be borne in mind which is a known complication with regular use of ICS.
Figure 2. Initial pharmacological treatment in COPD as per ABCD scheme
Follow up of these patients should be done carefully ensuring all the aspects like avoidance of exposure, vaccination, self-management, education, compliance of pharmacotherapy, inhaler technique, level of symptoms and history of exacerbations to assess current clinical status and modify the treatment if necessary. Modification in treatment should be guided by the history obtained as per the flow chart in figure 2.
Firstly, the patient should be reviewed for symptoms and exacerbation risk. Then he should be assessed for appropriateness of ongoing therapy especially inhaler technique. Lastly, therapy should be adjusted if needed to achieve a better control as shown in figure 3.
Figure 3. Follow up of pharmacotherapy in COPD

Non-pharmacological treatment
In COPD, non-pharmacological interventions complement pharmacological therapy at every step. For overall improvement in outcome of COPD it is very important to give due weightage to both. It includes curtailing the risk factor i.e. smoking cessation, avoidance of biomass fuel exposure, regular vaccination, pulmonary rehabilitation, oxygen supplementation and ventilatory support and patient education on self-management, nutrition and end of life care (Table 3).
Table 3. Non-pharmacological management of COPD

Smoking cessation
Smoking is one of the most important risk factors in predominantly urban COPD in our country. All efforts should be taken towards smoking cessation to alter the natural history of disease. Avoidance of smoke exposure leads to improvement in rate of accelerated decline in lung function. Legislative action against smoking has helped by increasing strictness against this harmful habit. A well-established strategy with 5 A’s should be followed in all cases with patience.
- Ask every patient of COPD regarding smoking history by default
- Advise all the smokers to quit smoking in a strong and firm way
- Assess willingness in smoker for quit and analyse the rationale behind their decision
- Assist the patient in quitting by due guidance and support for the same
- Arrange for follow up of all such patients either in person or telephonically
In our country, biomass fuel exposure is a major contributor in COPD. Thus, all possible efforts to reduce such activities should be prioritised both indoors and outdoors.
Vaccination
Immunisation in COPD has proven to be helpful as to prevent recurrent infections and thereby exacerbations.
- Yearly influenza vaccination should be given to reduce worsening and deaths.
- Similarly, pneumococcal vaccination also is important. The 23-valent pneumococcal polysaccharide vaccine (PPSV23) and 13-valent conjugated pneumococcal vaccine (PCV-13) has shown evidence to prevent pneumonia in severe grade of COPD patients aged <65 years and serious invasive illness or bacteremia in age >65 years respectively.
Pulmonary rehabilitation
Pulmonary Rehabilitation (PR) has shown to reduce dyspnoea and effort tolerance in patients with COPD. Pulmonary rehabilitation is a comprehensive program targeting at physical activity, participation in day-to-day living, and psychological health. It also includes patient education regarding illness, coping techniques, nutrition, and regular vaccination. The program also helps to ensure compliance with the medication.
Regular PR has shown to improve functional exercising capacity in patients which improves their indoor and outdoor involvement in social or family matters. This in turn enhances quality of life in these patients. In the current scenario, all COPD patients must be enrolled in one such PR program as part of their therapy. Institution-based program is superior to home rehabilitation. However, as a continuation of care, those patients who are willing to and have a setup to continue the same set of exercises, should be identified and supported for the same.
PR reduces hospitalisation in patients who have had a recent exacerbation. Nutrition also plays a very important part in management of COPD. High protein, high carbohydrate with low fat diet should be taken.
Self-management
All patients need to be educated regarding the various aspects of COPD as a disease. They should be provided with a written action plan. Coping techniques are essential and should be taught so that they start managing themselves early on to reduce avoidable emergency department visits and even hospitalisation. It allows patients to participate in their own disease management.
Surgery and intervention
Surgical intervention in COPD should be restricted to those who have a localised pathology on CT scan like upper lobe emphysema or large bulla. With advanced disease, bronchoscopy guided endobronchial valves, lung coils, and vapour ablation can be done. These procedures help by reducing end-expiratory lung volume. In selected patients with very severe COPD progressing rapidly, who are not a candidate for lung volume reduction, lung transplantation can be considered if they fulfil the criteria.
Oxygen therapy and ventilatory support
In patients with severe resting hypoxemia, long term oxygen therapy should be initiated. However, for stable COPD patients with resting or exercise-induced moderate desaturation, long term oxygen should not be prescribed upfront. For those patients where blood gas analysis reveals evident chronic hypercapnia and a history of hospitalization for acute respiratory failure, long term non-invasive ventilatory support may be considered.
End of life care
For those terminally ill COPD patients who continue to suffer with distressing symptoms despite all possible therapies, palliative care should be initiated with the only goals of patient comfort and quality of life. Physicians must discuss with patients and their relatives regarding their views on resuscitation, advance directives and place of death preference.
Exacerbation
An exacerbation of chronic obstructive pulmonary disease (COPD) is defined as an acute worsening of respiratory symptoms that results in additional therapy. COPD exacerbations are complex events usually associated with increased airway inflammation, increased mucous production and marked gas trapping. These changes contribute to increased dyspnoea that is the key symptom of an exacerbation. Other symptoms include increased sputum purulence and volume, together with increased cough and wheezing. Exacerbations are mainly triggered by respiratory viral infections although bacterial infections and environmental factors such as pollution and ambient temperature may also initiate and/or amplify these events.
Exacerbations are classified as:
- Mild (treated with short acting bronchodilators only, SABDs)
- Moderate (treated with SABDs plus antibiotics and/or oral corticosteroids)
- Severe (patient requires hospitalization or visits the emergency room)
Severe exacerbations may also be associated with acute respiratory failure. A majority of exacerbations can be handled in outpatient care. However, those who require hospitalisation, should be classified into 3 categories namely- no respiratory failure, respiratory failure non-life threatening, and respiratory failure-life threatening.
Treatment of COPD exacerbation includes inhaled bronchodilators, systemic steroids, antibiotics, oxygen or ventilatory support, thromboprophylaxis as per clinical condition. Comorbidities especially associated cardiac disorders should also be optimised. Prevention of an exacerbation is of utmost importance which includes regular inhaled bronchodilators, ICS regimens, PDE4 inhibitors, long term macrolides, and vaccines. Pulmonary rehabilitation and smoking also help in prevention.
Click here to see references
Disclaimer- The views and opinions expressed in this article are those of the author's and do not necessarily reflect the official policy or position of M3 India.
The author, Dr. Ashok Mahashur, is a Senior Consultant in Respiratory Medicine at PD Hinduja Hospital, Mumbai and Consultant in Respiratory Medicine at Leelavati Hospital, Mumbai.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries