Evaluation of short stature in children: Clinic-based approach for general practitioners
M3 India Newsdesk Apr 22, 2020
Dr. SK Wangnoo, Dr. Ayesha Ahmad, and Dr. Asim Siddiqui discuss short stature in children, its evaluation and important learning points for general practitioners.
One of the most common presentations in any paediatric clinics, apart from colic and infections, are the parental complaints of short stature. It is imperative for any physician dealing with paediatric age group to have a basic idea about how to evaluate for growth disorders. This will not only avoid unnecessary evaluation but also give an indication for specialist referral. Early detection and diagnosis of the causes allows management of underlying medical conditions, optimising attainment of good health and most important, attainment of normal adult height. Unfortunately, in most of the cases, short stature in children is frequently not recognised in early childhood which decreases the opportunities for appropriate intervention. Endocrine aetiologies make up a small proportion of causes for short stature; most of them are treatable if recognised early.
What is short stature?
A child maybe considered to show growth retardation if her/his height falls below the 3rd percentile or below the 2SD of the median national standards. If the child is growing normally, but is excessively short for mid-parental or target height, he/she may still be regarded as having short stature. Also, if the growth velocity on successive height measurements has been demonstrated to be consistently below 25th centile over the preceding 6 to 12 months, an evaluation for growth retardation must be done.
In general, causes of short stature may be broadly divided into Physiological and Pathological.
Physiological Short Stature
- Familial
- Constitutional delay of growth and puberty
Pathological Short Stature
- Systemic Diseases – renal failure, anaemia, asthma, chronic infections etc
- Nutritional causes
- Endocrine disorders – growth hormone deficiency/insensitivity, hypothyroidism, Cushings etc.
- Intrauterine growth retardation
- Skeletal dysplasias and genetic causes
- Treatment of childhood malignancies
When to evaluate
Majority of the parental concerns regarding growth begin when the child is compared to the peers regarding the height issues. In our clinics, the common presenting complaints are that the child is not matching up in height compared to the peer group. Other causes including syndromic and genetic causes are relatively rare.
When growth slows and crosses the height centiles, even if still within the normal range on the growth chart, a pathological aetiology is more likely. Growth deceleration is said to occur when growth velocity is below the 5th percentile for age and gender (e.g. <5 cm/year after the age of 5 years) or a height drop across two or more percentiles on the growth chart. When growth velocity is abnormally decreased, height measurements will progressively fall across isobars, sometimes termed ‘falling off the curve’.
How to evaluate
As with any other organ system involvement, a detailed history supplemented by clinical examination gives a clue to underlying diagnosis.
The history should include ante-natal history, medications during gestation, birth weight and birth age, mode of delivery, consanguinity, family and social history. Specific pointers relating to organ system should also be enquired for. Clinical examination should be performed to look for skeletal dysplasias, features of nutritional deficiency and chronic diseases.
The growth monitoring or growth velocity may easily be done with the help of growth charts. They are easily available, can be marked by anyone and give a good idea about faltering growth. If used in a proper manner, unnecessary evaluation may be avoided, thus saving time, effort and also anxiety among the parents.
It is very important to measure the height in a proper manner because small variations can lead to an incorrect interpretation and subsequent evaluation. For measuring standing height, a horizontal headboard should move up and down a vertical support fixed to the wall. The child should be made to stand erect, with shoes and socks removed and heels, buttocks, back and occiput touching the vertical support.
For children below the age of 3 years, supine length can be taken. The infant should be measured using an infantometer. The lower segment is measured from symphysis pubis to the floor and upper segment measurement is obtained by difference of lower segment from height. If possible, the follow up measurements should be done by the same observer. Any conclusions regarding growth velocity should be drawn after a minimum of 6 months of observation.
It is important to remember that growth velocity varies from infancy to puberty. An average baby is expected to grow approximately 25 cm in the first year of life, half of that in second year, 6 – 7 cm in the third to fourth year and then 5 cm until the pubertal spurt. Growth velocity is not a smooth progression – it may be extremely low in one measurement interval and high in next interval measurements.
Bone age measurement gives an idea of skeletal maturity of the child. It is conventionally read from a radiograph of the left hand using either the Greulich & Pyle or Tanner & Whitehouse atlas. A combination of proper growth charting and bone age in most cases gives an idea of the pathological vs physiological growth defects.
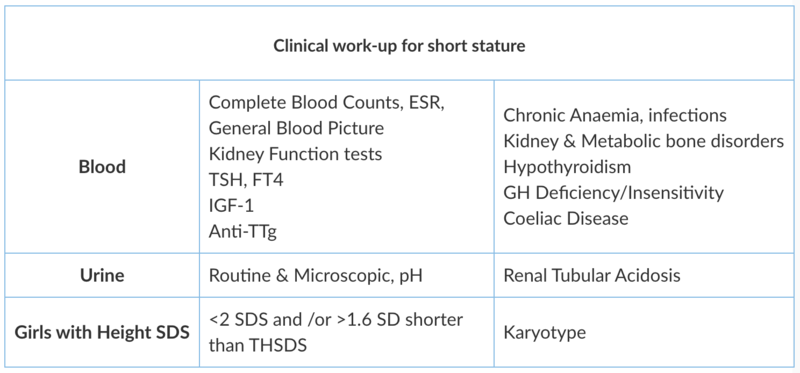
If the clinical work-up is suggestive of a cause for short stature, the appropriate tests may be embarked upon. These include:
Conclusion
Evaluation of short stature is an important and key clinical condition for the general practitioner to recognise. Short stature should be identified, diagnosed, and treated appropriately and without delay. The most useful tests in distinguishing the short normal child from one with a pathologic condition are accurate height measurements over time and calculation of the growth velocity.
Children who are short but growing at a normal growth velocity are healthy; a child whose growth velocity is decelerating irrespective of absolute height, needs thorough evaluation. Prompt recognition of the cause of short stature provides the best chance for a child to achieve an ideal health outcome as well as the potential to reach adult height.
Suggested Simplified Algorithm to evaluate Short Stature in a clinic

Learning Points
- Short stature is a complaint that practitioners commonly encounter in the outpatient setting.
- The key to diagnosing a cause is a detailed history, thorough physical exam, and meticulous height measurements over time.
- Attention to growth monitoring on growth chart gives a good idea of changes in height velocity which is helpful in planning out the investigations.
- Ancillary tests can be of benefit, but a differential diagnosis should be contemplated prior to ordering additional information. The therapeutic goal is to allow children to grow as tall as their genetic potential.
Disclaimer- The views and opinions expressed in this article are those of the author's and do not necessarily reflect the official policy or position of M3 India.
Dr. Subhash Kumar Wangnoo is a Senior Consultant Endocrinologist and Diabetologist for Obesity, Diabetes and Endocrinology (ACODE) in New Delhi.
Dr. Ayesha Ahmad is a Paediatric Endocrinologist at AMU, Aligarh.
Dr. Asim Siddiqui is a Senior Consultant Endocrinologist at Apollo Hospital, New Delhi.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries