Diabetes and Pregnancy: Dr. SK Wangnoo & Dr. KW Yadwad
M3 India Newsdesk Mar 17, 2020
Dr. SK Wangnoo and Dr. KW Yadwad, as part of an exclusive Endocrinology series, discuss diabetes and pregnancy- pregestational and GDM, goals of management and glycaemic targets.

Diabetes is a global health emergency. It was estimated that in 2017 there are 451 million (age 18 to 99 years) people with diabetes worldwide. These figures were expected to increase to 693 million by 2045. It was estimated that almost half of all people (49.7%) living with diabetes are undiagnosed. Moreover, there was an estimated 374 million people with impaired glucose tolerance (IGT) and it was projected that almost 21.3 million live births to women were affected by some form of hyperglycaemia in pregnancy.
In 2017,
- There were an estimated 204 million women (20 to 79 years) living with diabetes; the number projected to increase to 308 million by 2045
- 1 in 3 women with diabetes were of reproductive age
- 21.3 million or 16.2% of live births had some form of hyperglycaemia in pregnancy
- An estimated 85.1% were due to gestational diabetes
- 1 in 7 births was affected by gestational diabetes
The vast majority of cases of hyperglycaemia in pregnancy were in low- and middle-income countries.
Diabetes is a growing challenge in India with estimated 8.7% diabetic population in the age group of 20 and 70 years. With a higher proportion of younger population and increasing prevalence of diabetes mellitus among the young in India, there are rising trends in incidence and prevalence of both, the pregestational diabetes mellitus and gestational diabetes mellitus.
It is estimated that about 4 million women are affected by GDM in India, at any given time point. With all of its adversities and complications, diabetes in pregnancy possesses a significant challenge to the overall healthcare. It causes a burden on healthcare, maternal, and child health.
Diabetes mellitus is a syndrome of disordered metabolism with inappropriate hyperglycaemia due to an absolute or relative deficiency of insulin. There may also be a defect in insulin action (insulin resistance).
Diagnosis of diabetes mellitus
The American Diabetic Association (ADA) criteria for diagnosis of diabetes mellitus is as follows:
FPG ≥126 mg/dl (7.0 mmol/L). Fasting is defined as no caloric intake for at least 8 hours.
(OR)
2-hour PG ≥200 mg/dL (11.1 mmol/L) during OGTT. The test should be performed as described by the WHO, using a glucose load containing the equivalent of 75 g anhydrous glucose dissolved in water.
(OR)
A1C ≥6.5% (48 mmol/mol). The test should be performed in a laboratory using a method that is NGSP certified and standardised to the DCCT assay.
(OR)
In a patient with classic symptoms of hyperglycaemia (polydipsia, polyuria, unexplained weight loss or hyperglycaemic crisis, a random plasma glucose ≥200 mg/dL
In 2010 and 2013, respectively, the International Association of Diabetes and Pregnancy Study Groups (IADPSG) and the World Health Organization (WHO) reclassified hyperglycaemia in pregnancy into three groups to incorporate all aspects of the range of raised glucose that can increase pregnancy complications:
| WHO classification of hyperglycaemia in pregnancy | ||
| Known pre-gestational diabetes | Overt diabetes in pregnancy | Gestational Diabetes Mellitus (GDM) |
| Known diabetes | Diagnosed first time in pregnancy and expected to continue postnatally | Diagnosed first time in pregnancy and no permanent diabetes expected postnatally |
Pregestational diabetes
Pregestational diabetes implies a female already diagnosed as having diabetes prior to conception. It is observed in 1 to 2% of all pregnancies and 13 to 21% of diabetes in pregnancy. This includes women with type 1 diabetes and type 2 diabetes who have been diagnosed and treated prior to conception. Type 2 pregestational diabetes mellitus (PGDM) is now more common than type 1 as obesity prevalence and its associations are increasing in incidence.
Gestational Diabetes Mellitus (GDM)
It is defined as any degree of impaired glucose tolerance of with onset or first recognition during pregnancy. This does not exclude the possibility of some undiagnosed pregestational diabetes. GDM prevalence has been increasing in association with increase in obesity and is directly related to the prevalence of type 2 DM in a given population. GDM currently complicates up to 14% of all pregnancies and accounts for the vast majority of all cases of diabetes in pregnancy. Furthermore, 15 to 50% of women diagnosed with GDM will go on to be diagnosed with type 2 DM later in life.
Diagnosis of GDM
Carbohydrate metabolism during pregnancy
The most important reason why pregnancy exacerbates the diabetic tendency of asymptomatic women is the progressive increase in insulin resistance that occurs during pregnancy.
Diabetogenic effects of pregnancy
1. Insulin resistance
- Production of human placental lactogen
- Increased production of cortisol, estriol, and progesterone
- Increased insulin destruction by kidney and placenta
2. Increased lipolysis: The mother utilises fat for her caloric needs and saves glucose for foetal needs
3. Changes in gluconeogenesis: The foetus preferentially utilises alanine and other amino acids, depriving the mother of a major neogluconic source
Effects of diabetes on pregnancy
The great majority of women with carbohydrate intolerance during pregnancy do not have signs or symptoms. Unfortunately, carbohydrate intolerance during pregnancy causes significant increase in foetal and maternal morbidity.
Effects of diabetes on mother:
- Preeclampsia- Affects 10 to 25% of all pregnant diabetics
- Infections- High incidence of chorioamnionitis and postpartum endometritis
- Postpartum bleeding- High incidence due to exaggerated uterine distension
- Cesarean section- High incidence in pregnant diabetics
Effect of diabetes on foetus and newborn
Infants born to diabetic mothers (IDM) are at increased risk of complications which may be peri-conceptional, foetal and in the perinatal period which commences at 22 completed weeks of gestation (154 days) and ends 7 completed days after birth. GDM increases the risk of complications via a myriad of biological mechanisms. Spontaneous abortions and congenital anomalies may be induced in the first trimester. Excessive foetal growth, neonatal hypoglycaemia, jaundice, polycythemia and stillbirth are more common during the second and third trimesters.
Perinatal effects of maternal diabetes
1. Congenital malformations: Congenital anomalies in Infants of Diabetic Mothers (IDM) include,
Skeletal and central nervous system:
- Caudal regression syndrome
- Neural tube defects excluding anencephaly
- Anencephaly with or without herniation of neural elements
- Microcephaly
- Holoprosencephaly
Cardiac
- Transportation of the great vessels with or without ventricular septal defect
- Ventricular septal defects
- Coarctation of the aorta with or without ventricular septal or patent ductus arteriosus
- Single ventricle, hypoplastic left ventricle, pulmonic stenosis, and pulmonary valve atresia
- Atrial septal defects
- Cardiomegaly
- Double-outlet right ventricle and truncus arteriosus
Renal
- Hydronephrosis
- Renal agenesis
- Ureteral duplication
Gastrointestinal
- Duodenal atresia
- Anorectal atresia
- Small left colon syndrome
Other
- Single umbilical artery
2. Prematurity: A baby born at <37 weeks of gestation
3. Polyhydramnios
4. Large for gestational age: A large for gestation infant is defined as having a birth weight >90th percentile for gestational age.
5. Neonatal Hypoglycaemia: Defined as blood glucose level <40mg/dl or plasma glucose level <45 mg/dl in any infant regardless of gestational age.
6. Neonatal Hypocalcaemia: Defined as total serum calcium <7 mg/dL (1.75 mmol/L) or ionised calcium <4 mg/dL (1 mmol/L) for pre-term babies and <8 mg/dl(2 mmol/L) or ionised calcium <4.8 mg/dl (1.2 mmol/L) for term babies.
7. Polycythemia: Defined as a central venous hematocrit >65%.
8. Hyperbilirubinemia: Defined as serum total bilirubin >95th percentile on the hour specific Bhutani Nomogram.
Management of Diabetes in Pregnancy
Preconception Counseling
All women of childbearing age with diabetes should be counseled about the importance of strict glycaemic control prior to conception, risk of diabetic embryopathy, especially anencephaly, microcephaly, and congenital heart disease, that increases directly with elevations in HbA1c.
Spontaneous abortion is also increased in uncontrolled diabetes. Diabetes specific management should include A1C, thyroid stimulating hormone, creatinine, and urine albumin-to-creatinine ratio testing; review of the medication list for potentially teratogenic drugs (i.e. ACE inhibitors, statins); and referral for an ophthalmologic exam.
Screening
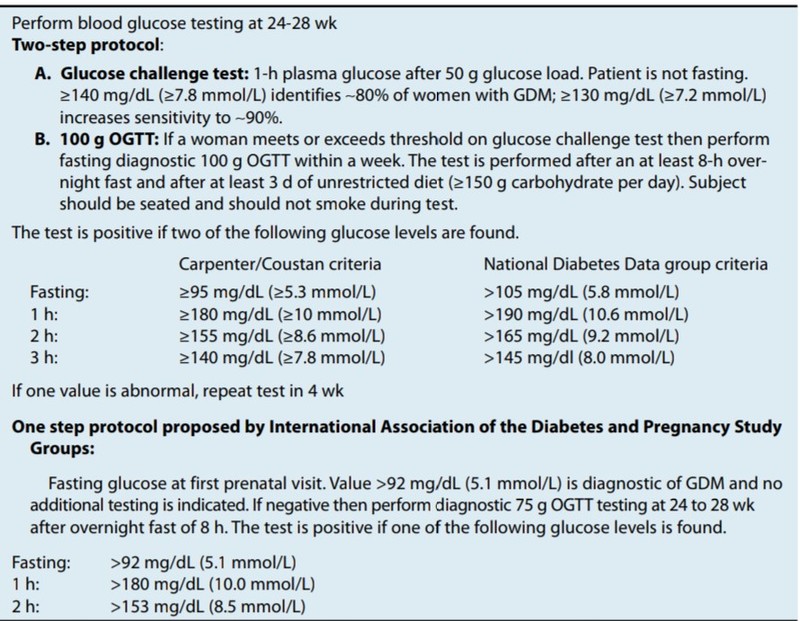
It should be performed between 24 and 28 weeks in those women not known to have glucose intolerance earlier in pregnancy. This evaluation is usually done in two steps. In the two step procedure, a 50 g oral glucose challenge test is followed by a diagnostic 100 g oral glucose tolerance test (OGTT) if initial results exceed the recommended plasma glucose concentration.
Goals of Management
- Optimal glyceamic control (no hypoglycaemia or hyperglycaemia)
- Optimal weight gain of mother and optimal foetal growth
- Optimal biological outcomes without psychosocial stress
Glycaemic targets in pregnancy
The goals for glycaemic control for GDM are based on recommendations from the Fifth International Workshop-Conference on Gestational Diabetes Mellitus and have the following targets for maternal capillary glucose concentrations:
- Preprandial- 95 mg/dL (5.3 mmol/L), and either,
- One-hour postmeal- 140 mg/dL (7.8 mmol/L) or two-hour postmeal- 120 mg/dL (6.7 mmol/L)
For women with pre-existing type 1 diabetes or type 2 diabetes who become pregnant, the following are recommended as optimal glycaemic goals if they can be achieved without excessive hypoglycaemia:
- Premeal glucose- 60 to 99 mg/dL (3.3 to 5.4 mmol/L)
- Peak postprandial glucose- 100 to 129 mg/dL (5.4 to 7.1 mmol/L)
- HbA1c <6.0%
Treatment of GDM
Treatment starts with medical nutrition therapy, exercise, and glucose monitoring aiming for the blood sugar targets. A total of 70 to 85% of women diagnosed with GDM can control GDM with lifestyle modification alone. Insulin is the preferred agent for management of diabetes in pregnancy. The physiology of pregnancy requires frequent titration of insulin to match changing requirements.
In the first trimester, there is often a decrease in total daily dose of insulin. In the second trimester, rapidly increasing insulin resistance requires weekly or biweekly increase in insulin dose to achieve glycaemic targets. In general, a small proportion of the total daily dose should be given as basal insulin and a greater proportion as prandial insulin. Due to the complexity of insulin management in pregnancy, referral to a specialised center is recommended if this resource is available.
All insulins are pregnancy category B except for glargine and glulisine, which are labeled C. Frequent hypoglycaemia can be associated with intrauterine growth restriction. In addition, rapid implementation of tight glycaemic control in the setting of retinopathy is associated with worsening of retinopathy. Insulin resistance drops rapidly with delivery of the placenta, and women become very insulin sensitive, requiring much less insulin than in the prepartum period.
Pregestational type 2 diabetes is often associated with obesity. Recommended weight gain during pregnancy for overweight women is 15 to 25 lb and for obese women is 10 to 20 lb. Glycaemic control is often easier to achieve in type 2 diabetes than in type 1 diabetes, but hypertension and other comorbidities often render pregestational type 2 diabetes as high or higher risk than pregestational type 1 diabetes.
All women should be supported in attempts to nurse their babies, given immediate nutritional and immunological benefits of breastfeeding for the baby; there may also be a longer-term metabolic benefit to both mother and offspring. GDM may represent preexisting undiagnosed type 2 diabetes, women with GDM should be screened for persistent diabetes or prediabetes at 6 to 12 weeks postpartum using non-pregnancy criteria and every 1 to 3 years thereafter depending on other risk factors.
Interpregnancy or postpartum weight gain is associated with increased risk of adverse pregnancy outcomes in subsequent pregnancies and earlier progression to type 2 diabetes. Both metformin and intensive lifestyle intervention prevent or delay progression to diabetes in women with a history of GDM.
In patients with type 1 diabetes, insulin sensitivity increases in the immediate postpartum period and then returns to normal over the following 1 to 2 weeks, and many women will require significantly less insulin at this time than during the prepartum period. Breastfeeding may cause hypoglycaemia, which may be ameliorated by consuming a snack (such as milk) prior to nursing.
To conclude, management of diabetes in pregnancy involves a holistic approach involving adequate glycaemic control with lifestyle modification, nutrition, and insulin. Patient and family education is of paramount importance in easing the psychosocial stress associated. Diabetes in pregnancy should be rigorously managed towards the ultimate objective of a healthy mother with a healthy baby.
Disclaimer- The views and opinions expressed in this article are those of the author's and do not necessarily reflect the official policy or position of M3 India.
The writer, Dr. Subhash Kumar Wangnoo is a Senior Consultant Endocrinologist and Diabetologist at Apollo Centre for Obesity, Diabetes and Endocrinology (ACODE) in New Delhi.
The write, Dr. Khwajamuhammedusman W Yadwad is an Endocrine Fellow at Apollo Centre for Obesity, Diabetes and Endocrinology (ACODE) in New Delhi.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries